Abstract
Autoimmune encephalitis represents a potentially treatable immune-mediated condition that is being more frequently recognized. Prompt immunotherapy is a key factor for the management of autoimmune encephalitis. First-line treatments include intravenous steroids, plasma exchange, and intravenous immunoglobulins, which can be combined in most severe cases. Rituximab and cyclophosphamide are administered as second-line agents in unresponsive cases. A minority of patients may still remain refractory, thus representing a major clinical challenge. In these cases, treatment strategies are controversial, and no guidelines exist. Treatments proposed for refractory autoimmune encephalitis include (1) cytokine-based drugs (such as tocilizumab, interleukin-2/basiliximab, anakinra, and tofacitinib); (2) plasma cell-depleting agents (such as bortezomib and daratumumab); and (3) treatments targeting intrathecal immune cells or their trafficking through the blood–brain barrier (such as intrathecal methotrexate and natalizumab). The efficacy evidence of these drugs is mostly based on case reports or small case series, with few reported controlled studies or systematic reviews. The aim of the present review is to summarize the current evidence and related methodological issues in the use of these drugs for the treatment of refractory autoimmune encephalitis.
Similar content being viewed by others
A minority of patients with autoimmune encephalitis may remain refractory even to second-line therapies and they represent a major clinical challenge. In these cases, treatment strategies are controversial, and no guidelines exist. |
Treatments proposed for refractory autoimmune encephalitis include cytokine-based drugs, plasma cell-depleting agents, and treatments targeting intrathecal immune cells or their trafficking through the blood–brain barrier. |
The evidence of efficacy of these treatments is mostly based on case reports or small case series, controlled studies and systematic reviews are rare. |
1 Introduction
In recent years, the advances in the diagnostic assays and the recognition of novel clinical syndromes have helped to define the new emerging field of autoimmune neurology. Autoimmune encephalitides (AEs) represent a broad spectrum of immune-mediated and potentially treatable disorders that are currently being more frequently recognized. The underlying pathogenesis of these conditions is related to the presence of pathogenic antibodies directed against neuronal cell surface antigens or to a T-cell-mediated process in paraneoplastic disorders associated with non-pathogenic antibodies directed against intracellular targets [1, 2].
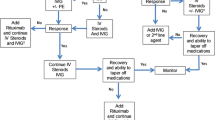
Prompt immunotherapy [3, 4] is the mainstay of AEs treatment and includes first-line and second-line medications. Intravenous steroids [5, 6], intravenous immunoglobulins [7], and plasma exchange [8] represent first-line immunotherapies. These treatments may be administered sequentially or in association, in particular steroids and plasma exchange/intravenous immunoglobulins, in the case of rapidly progressive or severe symptoms at onset [9].
Second-line treatment should be subsequently administered in the case of no clinical improvement after 2–4 weeks of first-line immunotherapy [10]. Rituximab and cyclophosphamide are the most frequently administered treatments. In particular, cyclophosphamide is preferred over rituximab in paraneoplastic disorders, as it depletes T cells, crosses the blood–brain barrier (BBB), and may be part of the oncological treatment scheme [11]. Antibody specificity also influences treatment choices, as demonstrated by the different response to rituximab in patients with antibodies to N-methyl-d-aspartate receptor (anti-NMDAR) [10], Leucine-rich Glioma Inactivated 1 (LGI1) [12,13,14,15], or Contactin-associated protein-like 2 (CASPR2) [16].
A minority of patients will not respond to second-line treatments [4] with consequent high disability and prolonged admissions to intensive care units. Despite the lack of a proper definition, these patients are labeled as “refractory” and the therapeutic approach is still debated [9]. Indeed, there are no phase III clinical trials for third-line agents and the evidence mostly relies on small studies or case series/reports.
Different molecules have been proposed as potential treatments for refractory AEs and include plasma cell-depleting agents (bortezomib, daratumumab), cytokine-based drugs (interleukin-2/basiliximab, tocilizumab, anakinra, tofacitinib), and treatments targeting intrathecal immune cells or their trafficking through the BBB (intrathecal methotrexate, natalizumab).
The aim of this narrative review is to summarize and discuss therapeutic options for refractory AEs (data are summarized in Table 1 and Fig. 1). Relevant studies were identified through a PubMed search (“refractory autoimmune encephalitis”) and by cross-referencing all significant results.
Mechanisms of action of therapeutic options applied to refractory autoimmune encephalitis. These drugs may be classified as plasma cell-depleting agents (in red), cytokine-based drugs (in black), and treatments targeting intrathecal immune cells or their trafficking through the blood–brain barrier (in orange). The lines depicted in the figure, as well as the description in italics, indicate the molecular and cellular target of each treatment. Dashed lines indicate that the drug affects peripheral immune cells, whilst solid lines indicate that treatment affects intrathecal immune cells or their trafficking across the blood–brain barrier. CD cluster of differentiation, IL interleukin, JAK Janus kinase
2 Cytokine-Based Drugs
2.1 Tocilizumab
Tocilizumab is a humanized monoclonal antibody that blocks interleukin-6 signal transduction, which has a pivotal importance in the stimulation of both T and B cells. Tocilizumab has been successfully used in neuromyelitis optica spectrum disorders and, more recently, in patients affected by myelin oligodendrocyte glycoprotein-associated disorder [17]. Similarly, a recent phase III trial has proved the efficacy of satralizumab, a recycling antibody against interleukin-6, in neuromyelitis optica spectrum disorders [18].
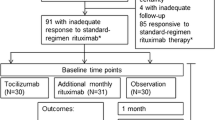
As for AEs, escalation treatment with tocilizumab was associated with better outcomes in terms of modified rankin scale (mRS) at every timepoint when compared with control groups including patients who received rituximab or were treated with first-line immunotherapies only [19]. This study included seronegative (n = 60), anti-NMDAR (n = 26), LGI1 (n = 3), and amphiphysin (n = 2) positive cases. At the last follow-up, 60% of patients treated with tocilizumab had a mRS ≤ 2 in comparison to 22% and 20% of patients receiving rituximab or no treatment, respectively. The authors suggest escalating to tocilizumab within 1 month from rituximab failure. Side effects were mainly related to neutropenia (about 10%), which led to drug discontinuation in one patient, while no infections were reported.
An additional study focused on anti-NMDAR encephalitis and analyzed the efficacy of the rapid escalation of teratoma removal, steroids, intravenous immunoglobulins, rituximab, and tocilizumab (T-SIRT protocol) [20]. Notably, patients who completed the T-SIRT protocol within 1 month had a more prominent improvement, and tocilizumab led to more favorable outcomes in comparison to steroids and intravenous immunoglobulins, steroids, intravenous immunoglobulins, or rituximab. The most common related side effects were neutropenia and urinary tract infections.
Of note, tocilizumab was associated with a prompt improvement even after prolonged and severe disease in a heterogeneous cohort of pediatric patients with immune-mediated disorders (including autoimmune neuropsychiatric disorders associated with streptococcal infections, rheumatic fever associated with encephalopathy, and glutamic acid decarboxylase-related ataxia with cognitive impairment) [21]. Finally, a prompt and sustained clinical response accompanied by a reduction in antibody titers was observed in two patients with CASPR2 and one patient with glutamic acid decarboxylase 65-associated encephalitis treated with tocilizumab as an upfront treatment [22,23,24].
2.2 Interleukin-2/Basiliximab
Interleukin-2 acts on T-regulatory and effector cells by promoting proper functioning, survival, and differentiation. The threshold of activation is lower for regulatory cells compared with effector cells, thus low doses of interleukin-2 may selectively affect T-regulatory cells without stimulating effector cells [25].
A low dose of subcutaneous interleukin-2 has been reported as a treatment for refractory AEs in a retrospective study including ten patients (four with anti-NMDAR and six with seronegative encephalitis) receiving a median of four treatment cycles [26]. All these patients had already received rituximab and tocilizumab. Six patients, including all anti-NMDAR encephalitides, improved, most of them after at least two cycles. Side effects rarely occurred and included fever (n = 1) and neutropenia responsive to colony-stimulating factors (n = 1). The potential benefit of blocking interleukin-2 signaling with a predominant effect on T-effector cells has been confirmed by the improvement of a patient with glutamic acid decarboxylase 65-associated limbic encephalitis after treatment with intravenous basiliximab, a monoclonal antibody directed against the alpha chain of the interleukin-2 receptor [27].
2.3 Anakinra
Anakinra, an interleukin-1 receptor antagonist, acts by inhibiting the response to interleukin-1, which has a major role in systemic inflammation. This drug, administered subcutaneously, has been successfully used for rheumatoid arthritis, periodic fevers, and autoinflammatory conditions.
Its administration led to a substantial benefit in a patient with seronegative limbic encephalitis characterized by new-onset refractory status epilepticus. Improvement was noted soon after the last dose of anakinra and progressed over the next 2 weeks [28]. These results were not confirmed in a heterogeneous case series of autoinflammatory nervous system disorders, where improvement was noted in patients with an acute disseminated encephalomyelitis-like phenotype but not in one case of seronegative autoimmune encephalitis [29, 30]. Notably, anakinra was tested in a rodent passive transfer animal model of anti-NMDAR encephalitis that developed seizure and cognitive disturbances [31]. Treated mice experienced a prompt (24–48 h after) reduction in seizures, memory improvement, and a reduction in the markers of activated microglia and astrogliosis.
2.4 Tofacitinib
Janus kinases 1 and 3 regulate the expression of both type I and II interferon, as well as the interleukin family receptors. These kinases are inhibited by tofacitinib, an orally administered drug that is able to penetrate the BBB.
The efficacy of tofacitinib has been evaluated in a case series [32] that included eight patients (anti-NMDAR encephalitis n = 2, glutamic acid decarboxylase 65 n = 1, myelin oligodendrocyte glycoprotein-associated disorder n = 1, seronegative n = 4). All patients received rituximab and some cases also tocilizumab, infliximab (a monoclonal antibody targeting tumor necrosis factor), or interleukin-2 previously.
A good response was observed in two patients (complete resolution of refractory meningoencephalitis with a significant reduction in both mRS and Clinical Assessment Scale in Autoimmune Encephalitis score; cessation of new-onset refractory status epilepticus associated with myelin oligodendrocyte glycoprotein antibodies), a partial response with no further disease progression in three cases, and an unclear response in three cases. The cytokine profile did not differ according to the treatment response.
Side effects were uncommon and included mild nausea and neutropenia. In previous studies, demyelinating lesions have been reported as a side effect of tofacitinib [33].
3 Plasma Cell-Depleting Agents
3.1 Bortezomib
The 26S proteasome inhibitor bortezomib represents a mainstay in the treatment of multiple myeloma as it disrupts the survival of long-lived plasma cells [34]. The rationale of employing bortezomib in immune-mediated disorders is that plasma cells are relatively unaffected by rituximab, as they do not express CD20, and thus long-lived plasma cells may continue to secrete pathogenic autoantibodies despite complete B-cell depletion [35]. Bortezomib has been used in other autoimmune conditions such as systemic lupus erythematosus [36] and neuromyelitis optica spectrum disorders [19]. Bortezomib may be administered either intravenously or subcutaneously.
As for AEs, treatment with bortezomib has been nearly exclusively reported in patients with anti-NMDAR encephalitis, in particular, in cases with severe disability who required a prolonged intensive care unit stay at the time of treatment administration, and in one patient with CASPR2 encephalitis, unsuccessfully treated with three cycles [38, 39]. In the reported single cases or small case series, bortezomib was used after failure of conventional or unconventional treatments such as cyclophosphamide, rituximab, interleukin-2, or tocilizumab [39,40,41,42,43,44,45,46,47,48,49,50,51,52]. As expected, bortezomib has been shown to deplete antibody-secreting cells that were not susceptible to rituximab [52].
Although most of these studies report the efficacy of bortezomib, one prospective study [51] failed to demonstrate the influence of bortezomib on disease course when compared to a control untreated historical cohort. This could be partially explained by the lack of proper BBB penetration by bortezomib, also most of these patients had high-titer cerebrospinal fluid (CSF) anti-NMDAR antibodies, which are also considered a poor prognostic factor. According to a systematic review, improvement can occur in 55.2% of patients after a median of two (one to six) bortezomib cycles. Of note, outcome is not influenced by a paraneoplastic origin but is affected by lower CSF anti-NMDAR onset titers and by the decrease of serum titers after treatment [53].
Side effects occur in 37.9% of patients, more commonly in cases with unfavorable outcomes at the last follow-up. Hematological side effects were the most frequent, followed by infectious and gastrointestinal side effects. A single case with reversible neuropathy has also been described [53].
3.2 Daratumumab
Daratumumab is a monoclonal antibody directed against CD38, which is also used in the setting of multiple myeloma [54]. The expression of CD38 in both plasma cells and T cells widens the potential benefit of daratumumab in comparison to other plasma cell-depleting drugs. Moreover, daratumumab may be able to penetrate the BBB [55].
Intravenous administration of daratumumab has been reported in individual case reports, including one patient with CASPR2 [38] and two patients with anti-NMDAR encephalitis [56, 57]. Even though partial improvement was noticed, one patient remained severely disabled [56] and another improved slowly, reaching the nadir of disability 18 months after treatment [57]. Of note, one patient died of Gram-negative sepsis, highlighting the increased infection risk [38]. Notably, all treated patients had previously received multiple immunotherapies, including bortezomib.
An additional retrospective case series of patients with refractory autoimmune disorders included five patients with refractory AE of whom one was previously reported (two with antibodies against CASPR2, one with anti-NMDAR, two with antibodies against an unknown epitope) [58]. All these patients had previously received rituximab and one also bortezomib. Treatment with daratumumab led to a sustained improvement, even though both patients with CASPR2 encephalitis then deceased. Authors suggest administering six to eight cycles and continuing treatment according to individual responses. Clinical improvement usually occurred within 2–4 weeks but required >2 months in more severe cases. As for side effects, 4/5 patients reported infections and 1/5 had an increase of C reactive protein without fever. Moreover, hypogammaglobulinemia requiring monthly intravenous immunoglobulin administration may complicate treatment with daratumumab.
In patients with AEs, daratumumab induced a decrease of serum and CSF antibody titers, as well as a reduction in the serum neurofilament light chain concentration, suggesting its efficacy in reducing active axonal loss [20]. Intriguingly, CD38-positive T and natural killer cells decreased after treatment, suggesting an effect beyond plasma cell depletion.
4 Treatments Targeting Intrathecal Immune Cells or Their Trafficking Through the BBB
4.1 Intrathecal Methotrexate
Methotrexate inhibits the synthesis of folates, and its intrathecal administration, leading to a high CSF concentration with minimal systemic toxicity, has a relevant role in leptomeningeal seeding. Conversely, methotrexate has a poor penetration in brain parenchymal niches [59], where immune cells involved in the pathogenesis of autoimmune encephalitis reside, and the precise mechanism of action of intrathecal methotrexate remains elusive in this setting.
The efficacy of intrathecal methotrexate has been reported in individual series and in a pilot study including mainly patients with refractory anti-NMDAR encephalitis [60,61,62,63,64]. Most of the reported patients had a significant improvement that occurred early after the infusion (usually between 2 and 13 days) [60], even though some patients experienced a delayed improvement [61, 63]. Cerebrospinal fluid antibody titers decreased after treatment, being the persistence of high titers associated with a lack of improvement [62]. No major side effects were reported in those studies, but intrathecal methotrexate is associated with severe neurotoxicity, which may present with stroke-like symptoms, seizures, or encephalopathy [65].
4.2 Natalizumab
Natalizumab acts by blocking central nervous system immune cell trafficking through alpha4beta1 integrin, and it is commonly used in multiple sclerosis [66]. The efficacy of natalizumab has been reported in one case with Hu-associated limbic encephalitis [67] and in one case with anti-glial fibrillary acid protein antibody meningoencephalitis [68] occurring after exposure to cancer immunotherapy (nivolumab and ipilimumab and pembrolizumab, respectively).
A phase II trial of natalizumab in anti-Hu-associated paraneoplastic neurological syndromes [69] has been recently published and included four patients with limbic encephalitis. Three cycles of natalizumab led to disease stability in three patients and improvement in one patient. Overall, natalizumab ameliorated the disease course but was not superior to other treatments. Even though no cases were reported in the trial, the risk of progressive multifocal leukoencephalopathy after exposure to natalizumab should not be underestimated in patients with prior exposure to chemotherapy.
4.3 Ongoing Clinical Trials
Clinical trials related to the use of immunosuppressants in AEs are strikingly lacking and, as previously mentioned, evidence relies mainly on uncontrolled series. Even though, a randomized clinical trial on intravenous immunoglobulins administration in LGI1/CASPR2 patients has been recently published, the small sample size represents a major limiting factor in AEs trials [7, 70]. Regarding second-line therapies, the ExTINGUISH trial (NCT04372615) [71] is a phase II study that will assess the efficacy of inebilizumab, an anti-CD19 monoclonal antibody, in anti-NMDAR encephalitis. Inebilizumab can deplete CD19-positive, CD20-negative plasma blast and plasma cells, showing some potential advantages over rituximab. Moreover, a phase II trial (NCT04875975) of anti-neonatal Fc receptor rozanolixizumab is currently enrolling patients with LGI1 encephalitis with no prior exposure to immunosuppressants.
Finally, a multicenter randomized trial including adult patients with antibody-mediated AE unresponsive to rituximab is currently enrolling patients to assess the efficacy of bortezomib (NCT03993262) [72].
5 Discussion
The evidence of treatment efficacy in refractory AE is still largely anecdotical and many questions remain still unsolved. Some major potential limitations and biases in the interpretation of these studies must be mentioned.
The first and most notable is that most of these studies include small series or individual case reports, and prospective or controlled studies are rare. The heterogeneity in terms of clinical syndromes, antibody specificity (i.e., most of the patients treated with tocilizumab and nearly all patients who received bortezomib were affected by anti-NMDAR encephalitis; one patient after tofacitinib treatment was affected by myelin oligodendrocyte glycoprotein-associated disorder, which differs from other AEs in terms of pathogenesis), previous treatments, follow-up duration, and treatment regimens (administration route, number of cycles) also hinders the proper evaluation of treatment efficacy and the comparison among different third-line therapies. Moreover, most of these studies used mRS as a reported main outcome, rather than other disease-severity scales, such as the Clinical Assessment Scale in Autoimmune Encephalitis score [73], which may be more sensitive to detect subtle improvements in severely affected patients.
Another limitation is that clinical improvement, in some patients, might reflect the expected natural disease course rather than treatment response, as a delayed improvement may be seen in patients with severe AE (particularly in those with anti-NMDAR antibodies) regardless of treatments [74]. However, some cases showed a dramatic response temporally related to third-line treatments [40, 43, 60].
The lack of a proper control group in most of the studies performed, which are composed mainly of uncontrolled case reports/series, represents another relevant limitation, which makes it impossible to distinguish a spontaneous improvement versus a treatment response. Moreover, when control groups were included, some relevant biases were introduced, such as being an historical cohort [51] or including patients not escalating to second-line therapies, possibly indicative of a less severe disease course [19].
Moreover, reporting biases (i.e., reporting only patients who improve with a specific third-line therapy) represents a major issue when dealing predominantly with case reports or series and, finally, most of these studies have a short follow-up duration after third-line treatments. The lack of a proper follow-up is extremely relevant (a) to properly determine a disease prognosis, (b) to identify a relapsing course, and (c) to guide long-term management. Indeed, there are currently few data regarding long-term immunotherapy and treatment de-escalation in patients with refractory AEs [53, 75].
Taking into account all these factors, tocilizumab and bortezomib seem to have the most compelling, even though limited, evidence of efficacy based on prospective and retrospectively controlled studies [9]. Of note, the administration of tocilizumab was constantly associated with a clinical improvement in different studies, whereas a negative-result study [51] and the incapability of crossing the BBB, which is relevant for these conditions often associated with intrathecal antibodies, pose some concerns regarding the efficacy of bortezomib. Moreover, treatment with bortezomib has been reported mostly in patients with anti-NMDAR encephalitis, whilst tocilizumab has been successfully applied in sporadic cases with different autoantibodies. Data regarding a direct comparison between the two treatments are not available yet, thus the choice should be tailored to each individual patient. Escalation therapy should be performed as soon as possible, within 1 month according to studies performed using tocilizumab [19, 20], although an improvement may be seen even in the case of a late escalation to third-line therapies [39]. Side effects of these two drugs are predominantly of hematological or infectious origin and should always be considered, especially in patients receiving multiple immunosuppressants with different mechanisms of action in a relatively short period of time.
The efficacy evidence of the remaining treatments herein reviewed is still extremely limited, although promising, in particular for those drugs acting on the intrathecal immune response (such as intrathecal methotrexate, tofacitinib, and possibly daratumumab), which may be implied in the refractoriness of these conditions and may be unaffected by some second-line or third-line therapies. These medications should be considered only after tocilizumab and/or bortezomib failure as (a) some patients did not improve after tocilizumab/bortezomib, but improved after daratumumab [56,57,58] or tofacitinib [32], (b) the evidence of efficacy of these drugs is mostly anecdotal and, on the contrary, the effects of bortezomib and tocilizumab rely only on case reports/series lacking a control group, and (c) these drugs may be associated with relevant side effects that should not be overlooked. Among the analyzed treatments, natalizumab may represent a safe and effective treatment for refractory T-cell-mediated encephalitides, such as those associated with cancer immunotherapy or intracellular antibodies [67,68,69].
6 Conclusions
Refractory AE poses relevant clinical challenges and the current evidence of therapeutic options is overall unsatisfactory, as it is mostly based on case reports/series or a few controlled studies with relevant biases. To date, tocilizumab seems to be the most effective option in refractory cases, whereas bortezomib could be useful, but more evidence is mandatory. The evidence for other treatments mostly relies on a small uncontrolled number of cases and no definite recommendations may be drawn.
Several methodological issues should be taken into account in further studies, in particular (a) the lack of an unique definition of refractoriness; (b) the necessity of a control group with a consistent follow-up to determine treatment efficacy and rule out spontaneous improvement; (c) the use of dedicated clinical scales, more sensible to evaluate subtle improvements, rather than mRS; (d) the inclusion of specific clinical phenotypes and antibody specificities in clinical trials; (e) a consistent evaluation of antibody titers, in both serum and CSF, to evaluate systemic and intrathecal treatment responses; and (f) the evaluation of potential biomarkers, such as neurofilament light chain, which may help in treatment decisions [76].
References
Dubey D, Pittock SJ, Kelly CR, McKeon A, Lopez-Chiriboga AS, Lennon VA, et al. Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann Neurol. 2018;83:166–77.
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15:391–404.
Irani SR, Stagg CJ, Schott JM, Rosenthal CR, Schneider SA, Pettingill P, et al. Faciobrachial dystonic seizures: the influence of immunotherapy on seizure control and prevention of cognitive impairment in a broadening phenotype. Brain. 2013;136:3151–62.
Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-N-methyl-D-aspartate (NMDA) receptor encephalitis. Lancet Neurol. 2014;12:157–65.
Thompson J, Bi M, Murchison AG, Makuch M, Bien CG, Chu K, et al. The importance of early immunotherapy in patients with faciobrachial dystonic seizures. Brain. 2018;141:348–56.
Rodriguez A, Klein CJ, Sechi E, Alden E, Basso MR, Pudumjee S, et al. LGI1 antibody encephalitis: acute treatment comparisons and outcome. J Neurol Neurosurg Psychiatry. 2022;93:309–15.
Dubey D, Britton J, McKeon A, Gadoth A, Zekeridou A, Lopez Chiriboga SA, et al. Randomized placebo-controlled trial of intravenous immunoglobulin in autoimmune LGI1/CASPR2 epilepsy. Ann Neurol. 2020;87:313–23.
Jacob S, Mazibrada G, Irani SR, Jacob A, Yudina A. The role of plasma exchange in the treatment of refractory autoimmune neurological diseases: a narrative review. J Neuroimmune Pharmacol. 2021;16:806–17. https://doi.org/10.1007/s11481-021-10004-9.
Abboud H, Probasco JC, Irani S, Ances B, Benavides DR, Bradshaw M, et al. Autoimmune encephalitis: Proposed best practice recommendations for diagnosis and acute management. J Neurol Neurosurg Psychiatry. 2021;92:757–68.
Zuliani L, Nosadini M, Gastaldi M, Spatola M, Iorio R, Zoccarato M, et al. Management of antibody-mediated autoimmune encephalitis in adults and children: literature review and consensus-based practical recommendations. Neurol Sci. 2019;40:2017–30.
Nosadini M, Eyre M, Molteni E, Thomas T, Irani SR, Dalmau J, et al. Use and safety of immunotherapeutic management of N-methyl-D-aspartate receptor antibody encephalitis: a meta-analysis. JAMA Neurol. 2021;78:1333–44.
Irani SR, Gelfand JM, Bettcher BM, Singhal NS, Geschwind MD. Effect of rituximab in patients with leucine-rich, glioma-inactivated 1 antibody-associated encephalopathy. JAMA Neurol. 2014;71:896–900.
Brown JWL, Martin PJ, Thorpe JW, Michell AW, Coles AJ, Cox AL, et al. Long-term remission with rituximab in refractory leucine-rich glioma inactivated 1 antibody encephalitis. J Neuroimmunol. 2014;271:66–8. https://doi.org/10.1016/j.jneuroim.2014.03.012.
Cheli M, Dinoto A, Tommasini V, Ajčević M, Stella G, Catalan M, et al. Efficacy of rituximab on seizure control and cognitive symptoms in leucine-rich, glioma-inactivated 1 (LGI1) limbic encephalitis: a high-density electroencephalography case study. Epileptic Disord. 2020;22:678–82.
Markovic I, Basic S, Devedjija S. Aggressive anti-LGI1 encephalitis defeated by one cycle of intravenous rituximab: a case report. Neurol Sci. 2020;41:1949–50.
Thaler FS, Zimmermann L, Kammermeier S, Strippel C, Ringelstein M, Kraft A, et al. Rituximab treatment and long-term outcome of patients with autoimmune encephalitis: real-world evidence from the GENERATE Registry. Neurol Neuroimmunol Neuroinflamm. 2021;8: e1088.
Ringelstein M, Ayzenberg I, Lindenblatt G, Fischer K, Gahlen A, Novi G, et al. Interleukin-6 receptor blockade in treatment-refractory MOG-IgG-associated disease and neuromyelitis optica spectrum disorders. Neurol Neuroimmunol Neuroinflamm. 2022;9: e1100. https://doi.org/10.1212/NXI.0000000000001100.
Yamamura T, Kleiter I, Fujihara K, Palace J, Greenberg B, Zakrzewska-Pniewska B, et al. Trial of satralizumab in neuromyelitis optica spectrum disorder. N Engl J Med. 2019;381:2114–24.
Lee WJ, Lee ST, Moon J, Sunwoo JS, Byun JI, Lim JA, et al. Tocilizumab in autoimmune encephalitis refractory to rituximab: an institutional cohort study. Neurotherapeutics. 2016;13:824–32. https://doi.org/10.1007/s13311-016-0442-6.
Lee WJ, Lee ST, Shin YW, Lee HS, Shin HR, Kim DY, et al. Teratoma removal, steroid, IVIG, rituximab and tocilizumab (T-SIRT) in anti-NMDAR encephalitis. Neurotherapeutics. 2021;18:474–87.
Randell RL, Adams AV, Van Mater H. Tocilizumab in refractory autoimmune encephalitis: a series of pediatric cases. Pediatr Neurol. 2018;86:66–8. https://doi.org/10.1016/j.pediatrneurol.2018.07.016.
Benucci M, Tramacere L, Infantino M, Manfredi M, Grossi V, Damiani A, et al. Efficacy of tocilizumab in limbic encephalitis with anti-CASPR2 antibodies. Case Rep Neurol Med. 2020;2020:1–5.
Krogias C, Hoepner R, Müller A, Schneider-Gold C, Schröder A, Gold R. Successful treatment of anti-Caspr2 syndrome by interleukin 6 receptor blockade through tocilizumab. JAMA Neurol. 2013;70:1056–9.
Jaafar F, Haddad L, Koleilat N, Sharara-Chami R, Shbarou R. Super refractory status epilepticus secondary to anti-GAD antibody encephalitis successfully treated with aggressive immunotherapy. Epilepsy Behav Rep. 2020;14: 100396. https://doi.org/10.1016/j.ebr.2020.100396.
Yu A, Zhu L, Altman NH, Malek TR. A Low interleukin-2 receptor signaling threshold supports the development and homeostasis of T regulatory cells. Immunity. 2009;30:204–17. https://doi.org/10.1016/j.immuni.2008.11.014.
Lim JA, Lee ST, Moon J, Jun JS, Park B-S, Byun JI, et al. New feasible treatment for refractory autoimmune encephalitis: low-dose interleukin-2. J Neuroimmunol. 2016;299:107–11. https://doi.org/10.1016/j.jneuroim.2016.09.001.
Widman G, Golombeck K, Hautzel H, Gross CC, Quesada CM, Witt J-A, et al. Treating a GAD65 antibody-associated limbic encephalitis with basiliximab: a case study. Front Neurol. 2015;6:167.
Choi CHO, Ma SHO, Ma KKY, Leung H, Mok VCT. Super-refractory status epilepticus in autoimmune encephalitis treated with interleukin-1 receptor antagonist, anakinra. Epileptic Disord. 2021;23:500–5.
Jang Y, Lee WJ, Lee HS, Chu K, Lee SK, Lee ST. Anakinra treatment for refractory cerebral autoinflammatory responses. Ann Clin Transl Neurol. 2022;9:91–7.
Jang Y, Woo KA, Lee ST, Park SH, Chu K, Lee SK. Cerebral autoinflammatory disease treated with anakinra. Ann Clin Transl Neurol. 2018;5:1428–33.
Taraschenko O, Fox HS, Zekeridou A, Pittock SJ, Eldridge E, Farukhuddin F, et al. Seizures and memory impairment induced by patient-derived anti-N-methyl-D-aspartate receptor antibodies in mice are attenuated by anakinra, an interleukin-1 receptor antagonist. Epilepsia. 2021;62:671–82.
Jang Y, Lee WJ, Lee HS, Chu K, Lee SK, Lee ST. Tofacitinib treatment for refractory autoimmune encephalitis. Epilepsia. 2021;62:e53–9.
Massoud F, Ismail II, Al-Hashel JY, Abboud H. CNS demyelination during tofacitinib therapy: first report. Mult Scler Relat Disord. 2020;46:2020–2.
Ito S. Proteasome inhibitors for the treatment of multiple myeloma. Cancers (Basel). 2020;12:265.
Sun B, Ramberger M, O’Connor KC, Bashford-Rogers RJM, Irani SR. The B cell immunobiology that underlies CNS autoantibody-mediated diseases. Nat Rev Neurol. 2020;16:481–92. https://doi.org/10.1038/s41582-020-0381-z.
Alexander T, Sarfert R, Klotsche J, Kühl AA, Rubbert-Roth A, Lorenz HM, et al. The proteasome inhibitior bortezomib depletes plasma cells and ameliorates clinical manifestations of refractory systemic lupus erythematosus. Ann Rheum Dis. 2015;74:1474–8.
Zhang C, Tian DC, Yang CS, Han B, Wang J, Yang L, et al. Safety and efficacy of bortezomib in patients with highly relapsing neuromyelitis optica spectrum disorder. JAMA Neurol. 2017;74:1010–2.
Scheibe F, Ostendorf L, Reincke SM, Prüss H, von Brünneck AC, Köhnlein M, et al. Daratumumab treatment for therapy-refractory anti-CASPR2 encephalitis. J Neurol. 2020;267:317–23. https://doi.org/10.1007/s00415-019-09585-6.
Scheibe F, Prüss H, Mengel AM, Kohler S, Nümann A, Köhnlein M, et al. Bortezomib for treatment of therapy-refractory anti-NMDA receptor encephalitis. Neurology. 2017;88:366–70.
Behrendt V, Krogias C, Reinacher-Schick A, Gold R, Kleiter I. Bortezomib treatment for patients with anti-N-methyl-D-aspartate receptor encephalitis. JAMA Neurol. 2016;73:1251–3. https://doi.org/10.1001/jamaneurol.2016.2588.
Sveinsson O, Granqvist M, Forslin Y, Blennow K, Zetterberg H, Piehl F. Successful combined targeting of B- and plasma cells in treatment refractory anti-NMDAR encephalitis. J Neuroimmunol. 2017;312:15–8. https://doi.org/10.1016/j.jneuroim.2017.08.011.
Kim LN, Edwards L, Goonetilleke N, Kane A, McDougall A, Calic Z. Bortezomib for the treatment of refractory anti-N-methyl-d-aspartate receptor encephalitis. Intern Med J. 2020;50:1591–2.
Schroeder C, Back C, Koc Ü, Strassburger-Krogias K, Reinacher-Schick A, Gold R, et al. Breakthrough treatment with bortezomib for a patient with anti-NMDAR encephalitis. Clin Neurol Neurosurg. 2018;172:24–6. https://doi.org/10.1016/j.clineuro.2018.06.005.
Keddie S, Crisp SJ, Blackaby J, Cox A, Coles A, Hart M, et al. Plasma cell depletion with bortezomib in the treatment of refractory N-methyl-d-aspartate (NMDA) receptor antibody encephalitis: rational developments in neuroimmunological treatment. Eur J Neurol. 2018;25:1384–8.
Zhang XT, Wang CJ, Wang BJ, Guo SG. The short-term efficacy of combined treatments targeting B cell and plasma cell in severe and refractory anti-N-methyl-D-aspartate receptor encephalitis: two case reports. CNS Neurosci Ther. 2019;25:151–3.
Cordani R, Micalizzi C, Giacomini T, Gastaldi M, Franciotta D, Fioredda F, et al. Bortezomib-responsive refractory anti-N-methyl-D-aspartate receptor encephalitis. Pediatr Neurol. 2020;103:61–4. https://doi.org/10.1016/j.pediatrneurol.2019.09.004.
Lazzarin SM, Vabanesi M, Cecchetti G, Fazio R, Fanelli GF, Volonté MA, et al. Refractory anti-NMDAR encephalitis successfully treated with bortezomib and associated movements disorders controlled with tramadol: a case report with literature review. J Neurol. 2020;267:2462–8. https://doi.org/10.1007/s00415-020-09988-w.
Turnbull MT, Siegel JL, Becker TL, Stephens AJ, Lopez-Chiriboga AS, Freeman WD. Early bortezomib therapy for refractory anti-NMDA receptor encephalitis. Front Neurol. 2020;11:1–6.
Govil-Dalela T, Datta I, Williams M. Refractory NMDA-receptor encephalitis in a teenager: a novel use of bortezomib. J Neuroimmunol. 2021;355:577565. https://doi.org/10.1016/j.jneuroim.2021.577565.
Karunaratne K, Ahrabian D, Monoghan B, Campion T, Yousry T, Lunn MP, et al. Bortezomib for anti-NMDAR encephalitis following daclizumab treatment in a patient with multiple sclerosis. BMJ Neurol Open. 2021;3:2018–21.
Shin YW, Lee ST, Kim TJ, Jun JS, Chu K. Bortezomib treatment for severe refractory anti-NMDA receptor encephalitis. Ann Clin Transl Neurol. 2018;5:598–605.
Wang T, Wang B, Zeng Z, Li H, Zhang F, Ruan X, et al. Efficacy and safety of bortezomib in rituximab-resistant anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis as well as the clinical characteristics: an observational study. J Neuroimmunol. 2021;354: 577527. https://doi.org/10.1016/j.jneuroim.2021.577527.
Dinoto A, Cheli M, Bratina A, Sartori A, Manganotti P. Bortezomib in anti-N-methyl-D-aspartate-receptor (NMDA-R) encephalitis: a systematic review. J Neuroimmunol. 2021;356: 577586. https://doi.org/10.1016/j.jneuroim.2021.577586.
Lokhorst HM, Plesner T, Laubach JP, Nahi H, Gimsing P, Hansson M, et al. Targeting CD38 with daratumumab monotherapy in multiple myeloma. N Engl J Med. 2015;373:1207–19.
Vercruyssen M, El Hachem G, Maerevoet M. The daratumumab crosses the blood brain barrier. Clin Lymphoma Myeloma Leuk. 2018;18:S289. https://doi.org/10.1016/j.clml.2018.07.229.
Lazzarin SM, Vabanesi M, Cecchetti G, Fazio R, Fanelli GF, Volonté MA, et al. Correction to: Refractory anti-NMDAR encephalitis successfully treated with bortezomib and associated movements disorders controlled with tramadol: a case report with literature review. J Neurol. 2021;268:741–2. https://doi.org/10.1007/s00415-020-10370-z (Journal of Neurology, (2020), 267, 8, (2462-2468), 10.1007/s00415-020).
Ratuszny D, Skripuletz T, Wegner F, Groß M, Falk C, Jacobs R, et al. Case report: daratumumab in a patient with severe refractory anti-NMDA receptor encephalitis. Front Neurol. 2020;11:1–5.
Scheibe F, Ostendorf L, Prüss H, Radbruch H, Aschman T, Hoffmann S, et al. Daratumumab for treatment-refractory antibody-mediated diseases in neurology. Eur J Neurol. 2022;29:1847–54.
Berg SL, Chamberlain MC. Systemic chemotherapy, intrathecal chemotherapy, and symptom management in the treatment of leptomeningeal metastasis. Curr Oncol Rep. 2003;5:29–40.
Eaton JE, Kleinholz-Owens P, Sriram S, Pawate S. Intrathecal methotrexate: another tool for the treatment of refractory autoimmune encephalitis: single institution cohort and literature review. J Neurol Sci. 2021;431: 120042. https://doi.org/10.1016/j.jns.2021.120042.
Liba Z, Sebronova V, Komarek V, Sediva A, Sedlacek P. Prevalence and treatment of anti-NMDA receptor encephalitis. Lancet Neurol. 2013;12:424–5. https://doi.org/10.1016/S1474-4422(13)70070-X.
Yang XZ, Zhu HD, Ren HT, Zhu YC, Peng B, Cui LY, et al. Utility and safety of intrathecal methotrexate treatment in severe anti-N-methyl-D-aspartate receptor encephalitis: a pilot study. Chin Med J (Engl). 2018;131:156–60.
Tatencloux S, Chretien P, Rogemond V, Honnorat J, Tardieu M, Deiva K. Intrathecal treatment of anti-N-methyl-D-aspartate receptor encephalitis in children. Dev Med Child Neurol. 2015;57:95–9.
Wang D, Wu Y, Ji Z, Wang S, Xu Y, Huang K, et al. A refractory anti-NMDA receptor encephalitis successfully treated by bilateral salpingo-oophorectomy and intrathecal injection of methotrexate and dexamethasone: a case report. J Int Med Res. 2020;48:300060520925666.
Bhojwani D, Sabin ND, Pei D, Yang JJ, Khan RB, Panetta JC, et al. Methotrexate-induced neurotoxicity and leukoencephalopathy in childhood acute lymphoblastic leukemia. J Clin Oncol. 2014;32:949–59.
Polman CH, O’Connor PW, Havrdova E, Hutchinson M, Kappos L, Miller DH, et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med. 2006;354:899–910. https://doi.org/10.1056/NEJMoa044397.
Hottinger AF, De Micheli R, Guido V, Karampera A, Hagmann P, Du Pasquier R. Natalizumab may control immune checkpoint inhibitor-induced limbic encephalitis. Neurol Neuroimmunol NeuroInflammation. 2018;5: e439.
Basin S, Perrin J, Michot JM, Lambotte O, Cauquil C. Severe anti-PD1-related meningoencephalomyelitis successfully treated with anti-integrin alpha4 therapy. Eur J Cancer. 2021;145:230–3.
Bastiaansen AEM, de Jongste AHC, de Bruijn MAAM, Crijnen YS, Schreurs MWJ, Verbeek MM, et al. Phase II trial of natalizumab for the treatment of anti-Hu associated paraneoplastic neurological syndromes. Neurooncol Adv. 2021;3:1–10. https://doi.org/10.1093/noajnl/vdab145/6377299.
Blackburn KM, Denney DA, Hopkins SC, Vernino SA. Low recruitment in a double-blind, placebo-controlled trial of ocrelizumab for autoimmune encephalitis: a case series and review of lessons learned. Neurol Ther. 2022;11:893–903. https://doi.org/10.1007/s40120-022-00327-x.
Day G, Titulaer M, Wong K-H, Torner J, Cudkowicz M, Coffey C, et al. The ExTINGUISH Trial: a phase-2B randomized placebo-controlled trial of inebilizumab in anti-NMDA receptor encephalitis (P5–1.004). Neurology. 2022;98:1651.
Wickel J, Chung HY, Platzer S, Lehmann T, Prüss H, Leypoldt F, et al. Generate-Boost: study protocol for a prospective, multicenter, randomized controlled, double-blinded phase II trial to evaluate efficacy and safety of bortezomib in patients with severe autoimmune encephalitis. Trials. 2020;21:1–12.
Lim JA, Lee ST, Moon J, Jun JS, Kim TJ, Shin YW, et al. Development of the clinical assessment scale in autoimmune encephalitis. Ann Neurol. 2019;85:352–8.
Rüegg S, Irani SR. The trouble with plasma cells. Neurology. 2017;88:340–1.
Abboud H, Probasco JC, Irani S, Ances B, Benavides DR, Bradshaw M, et al. Autoimmune encephalitis: Proposed recommendations for symptomatic and long-term management. J Neurol Neurosurg Psychiatry. 2021;92:897–907.
Mariotto S, Gajofatto A, Zuliani L, Zoccarato M, Gastaldi M, Franciotta D, et al. Serum and CSF neurofilament light chain levels in antibody-mediated encephalitis. J Neurol. 2019;266:1643–8. https://doi.org/10.1007/s00415-019-09306-z.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Open access funding provided by Università degli Studi di Verona within the CRUI-CARE Agreement.
Conflicts of interest/Competing interests
Alessandro Dinoto, Sergio Ferrari, and Sara Mariotto have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
AD: first draft of the manuscript, analysis and interpretation of data; SF: data interpretation, revised the manuscript for intellectual content; SM: data interpretation, manuscript draft revision, revised the manuscript for intellectual content.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Dinoto, A., Ferrari, S. & Mariotto, S. Treatment Options in Refractory Autoimmune Encephalitis. CNS Drugs 36, 919–931 (2022). https://doi.org/10.1007/s40263-022-00943-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00943-z