Abstract
Introduction
Clinical seizures and status epilepticus are frequent complications of encephalitis, can lead to depressed level of consciousness, and are associated with poor outcome. We sought to determine the frequency, risk factors, and clinical impact of electrographic seizures detected with continuing electroencephalography (cEEG) in patients with encephalitis and altered level of consciousness.
Methods
We retrospectively identified all patients with presumed or definite viral or autoimmune encephalitis who underwent cEEG monitoring at Henry Ford Hospital from January 2012 to October 2017. Clinical data and cEEG monitoring reports were abstracted and recorded. The primary outcome was electrographic seizures detected by cEEG.
Results
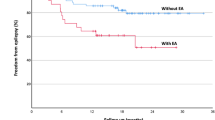
Of 1,735 patients who underwent a minimum of 12 h of cEEG monitoring, we identified 54 with a verified discharge diagnosis of encephalitis. Twenty-two of these patients (41%) had electrographic seizures on cEEG. Compared with encephalitis patients without seizures, electrographic seizures were associated with lower serum sodium levels (137 ± 5 vs 141 ± 7, P = 0.027) and more often were on antiepileptic therapy (100% vs 78%, P = 0.033) on the first day of monitoring. Seizures were also associated with a higher frequency of cortical imaging abnormalities (68% vs 28%, P = 0.005), lateralized periodic discharges (LPDs; 50% vs 16%, P = 0.014), delta background frequency (81% vs 45%, P = 0.010), low or suppressed voltage (96% vs 62%, P = 0.005), and focal slowing (86% vs 47%, P = 0.004). There was no association between electrographic seizures and clinical outcome at discharge.
Conclusion
Electrographic seizures occur in approximately 40% of patients with acute encephalitis. Low serum sodium, cortical imaging abnormalities, and on cEEG LPDs and background abnormalities are associated factors. The lack of association with short-term outcome suggests that with aggressive treatment, the clinical impact of electrographic seizures in encephalitis can be minimized.

Similar content being viewed by others
References
Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL, et al. The management of encephalitis: clinical practice guidelines by the infectious diseases society of America. Clin Infect Dis. 2008;47(3):303–27.
Vora NM, Holman RC, Mehal JM, Steiner CA, Blanton J, Sejvar J. Burden of encephalitis-associated hospitalizations in the United States, 1998–2010. Neurology. 2014;82(5):443–51.
Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10(12):835–44.
Thakur KT, Motta M, Asemota AO, Kirsch HL, Benavides DR, Schneider EB, et al. Predictors of outcome in acute encephalitis. Neurology. 2013;81(9):793–800.
Singh TD, Fugate JE, Rabinstein AA. The spectrum of acute encephalitis: causes, management, and predictors of outcome. Neurology. 2015;84(4):359–66.
Granerod J, Tam CC, Crowcroft NS, Davies NW, Borchert M, Thomas SL. Challenge of the unknown. A systematic review of acute encephalitis in non-outbreak situations. Neurology. 2010;75(10):924–32.
Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, Bitnun A, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis. 2013;57(8):1114–28.
Ney JP, van der Goes DN, Nuwer MR, Nelson L, Eccher MA. Continuous and routine EEG in intensive care: utilization and outcomes, United States 2005–2009. Neurology. 2013;81(23):2002–8.
Billakota S, Sinha SR. Utility of continuous EEG monitoring in noncritically lll hospitalized patients. J Clin Neurophysiol. 2016;33(5):421–5.
Carrera E, Claassen J, Oddo M, Emerson RG, Mayer SA, Hirsch LJ. Continuous electroencephalographic monitoring in critically ill patients with central nervous system infections. Arch Neurol. 2008;65(12):1612–8.
Mittal MK, Rabinstein AA, Hocker SE, Pittock SJ, Wijdicks EF, McKeon A. Autoimmune encephalitis in the ICU: analysis of phenotypes, serologic findings, and outcomes. Neurocrit Care. 2016;24(2):240–50.
Harris Paul A, Taylor Robert, Thielke Robert, Payne Jonathon, Gonzalez Nathaniel, Conde Jose G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391–404.
Hirsch LJ, LaRoche SM, Gaspard N, Gerard E, Svoronos A, Herman ST, et al. American clinical neurophysiology society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol. 2013;30(1):1–27.
Leitinger M, Beniczky S, Rohracher A, Gardella E, Kalss G, Qerama E, et al. Salzburg consensus criteria for non-convulsive status epilepticus—approach to clinical application. Epilepsy Behav. 2015;49:158–63.
Hirsch LJ, Claassen J, Mayer SA, Emerson RG. Stimulus-induced rhythmic, periodic, or ictal discharges (SIRPIDs): a common EEG phenomenon in the critically ill. Epilepsia. 2004;45(2):109–23.
Yoo JY, Rampal N, Petroff OA, Hirsch LJ, Gaspard N. Brief potentially ictal rhythmic discharges in critically ill adults. JAMA Neurol. 2014;71(4):454–62.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–4.
Sutter R, Kaplan PW, Cervenka MC, Thakur KT, Asemota AO, Venkatesan A, et al. Electroencephalography for diagnosis and prognosis of acute encephalitis. Clin Neurophysiol. 2015;126(8):1524–31.
Claassen J, Mayer SA, Kowalski RG, Emerson RG, Hirsch LJ. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology. 2004;62(10):1743–8.
Jette N, Claassen J, Emerson RG, Hirsch LJ. Frequency and predictors of nonconvulsive seizures during continuous electroencephalographic monitoring in critically ill children. Arch Neurol. 2006;63(12):1750–5.
Sutter R, Fuhr P, Grize L, Marsch S, Ruegg S. Continuous video-EEG monitoring increases detection rate of nonconvulsive status epilepticus in the ICU. Epilepsia. 2011;52(3):453–7.
Oddo M, Carrera E, Claassen J, Mayer SA, Hirsch LJ. Continuous electroencephalography in the medical intensive care unit. Crit Care Med. 2009;37(6):2051–6.
Friedman D, Claassen J, Hirsch LJ. Continuous electroencephalogram monitoring in the intensive care unit. Anesth Analg. 2009;109(2):506–23.
Sutter R, Stevens RD, Kaplan PW. Continuous electroencephalographic monitoring in critically ill patients: indications, limitations, and strategies. Crit Care Med. 2013;41(4):1124–32.
Misra UK, Kalita J. Seizures in encephalitis: predictors and outcome. Seizure. 2009;18(8):583–7.
Halawa I, Andersson T, Tomson T. Hyponatremia and risk of seizures: a retrospective cross-sectional study. Epilepsia. 2011;52(2):410–3.
Adrogue HJ, Madias NE. The challenge of hyponatremia. J Am Soc Nephrol. 2012;23(7):1140–8.
Overgaard-Steensen C, Ring T. Clinical review: practical approach to hyponatraemia and hypernatraemia in critically ill patients. Crit Care. 2013;17(1):206.
Rodriguez Ruiz A, Vlachy J, Lee JW, Gilmore EJ, Ayer T, Haider HA, et al. Association of periodic and rhythmic electroencephalographic patterns with seizures in critically ill patients. JAMA Neurol. 2017;74(2):181–8.
Gaspard N, Manganas L, Rampal N, Petroff OA, Hirsch LJ. Similarity of lateralized rhythmic delta activity to periodic lateralized epileptiform discharges in critically ill patients. JAMA Neurol. 2013;70(10):1288–95.
Punia V, Garcia CG, Hantus S. Incidence of recurrent seizures following hospital discharge in patients with LPDs (PLEDs) and nonconvulsive seizures recorded on continuous EEG in the critical care setting. Epilepsy Behav. 2015;49:250–4.
Garcia-Morales I, Garcia MT, Galan-Davila L, Gomez-Escalonilla C, Saiz-Diaz R, Martinez-Salio A, et al. Periodic lateralized epileptiform discharges: etiology, clinical aspects, seizures, and evolution in 130 patients. J Clin Neurophysiol. 2002;19(2):172–7.
Snodgrass SM, Tsuburaya K, Ajmone-Marsan C. Clinical significance of periodic lateralized epileptiform discharges: relationship with status epilepticus. J Clin Neurophysiol. 1989;6(2):159–72.
Chatrian GE, Shaw CM, Leffman H. The significance of periodic lateralized epileptiform discharges in EEG: an electrographic, clinical, and pathological study. Electroencephalogr Clin Neurophysiol. 1964;17:177–93.
Brigo F. Intermittent rhythmic delta activity patterns. Epilepsy Behav. 2011;20(2):254–6.
Foreman B, Claassen J, Abou Khaled K, Jirsch J, Alschuler DM, Wittman J, et al. Generalized periodic discharges in the critically ill: a case-control study of 200 patients. Neurology. 2012;79(19):1951–60.
Gaspard N, Gilmore EJ. Electroencephalography and evoked potentials. In: Louis ED, Mayer SA, Rowland LP, editors. Merritt’s neurology. 13th ed. Philadelphia: Wolters Kluwer; 2016. p. 206–15.
Swisher CB, Shah D, Sinha SR, Husain AM. Baseline EEG pattern on continuous ICU EEG monitoring and incidence of seizures. J Clin Neurophysiol. 2015;32(2):147–51.
Abend NS, Arndt DH, Carpenter JL, Chapman KE, Cornett KM, Gallentine WB, et al. Electrographic seizures in pediatric ICU patients: cohort study of risk factors and mortality. Neurology. 2013;81(4):383–91.
Chen JW, Wasterlain CG. Status epilepticus: pathophysiology and management in adults. Lancet Neurol. 2006;5(3):246–56.
DeLorenzo RJ, Pellock JM, Towne AR, Boggs JG. Epidemiology of status epilepticus. J Clin Neurophysiol. 1995;12(4):316–25.
Logroscino G, Hesdorffer DC, Cascino G, Annegers JF, Hauser WA. Short-term mortality after a first episode of status epilepticus. Epilepsia. 1997;38(12):1344–9.
Kang BS, Kim DW, Kim KK, Moon HJ, Kim YS, Kim HK, et al. Prediction of mortality and functional outcome from status epilepticus and independent external validation of STESS and EMSE scores. Crit Care. 2016;20:25.
Vooturi S, Jayalakshmi S, Sahu S, Mohandas S. Prognosis and predictors of outcome of refractory generalized convulsive status epilepticus in adults treated in neurointensive care unit. Clin Neurol Neurosurg. 2014;126:7–10.
Kaplan PW. Assessing the outcomes in patients with nonconvulsive status epilepticus: nonconvulsive status epilepticus is underdiagnosed, potentially overtreated, and confounded by comorbidity. J Clin Neurophysiol. 1999;16(4):341–52 (discussion 53).
Gaspard N, Hirsch LJ, LaRoche SM, Hahn CD, Westover MB. Interrater agreement for critical care EEG terminology. Epilepsia. 2014;55(9):1366–73.
Funding
This study was funded by Educational and Research Fund from Department of Neurology of Henry Ford Hospital. Tanuwong Viarasilpa has received funding from Siriraj Hospital, Mahidol University, Bangkok, Thailand. The funding sources had no role in the collection, analysis, or interpretation of the data.
Author information
Authors and Affiliations
Contributions
TV had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, performed data collection, analysis and interpretation, drafted and revised the manuscript. NP performed data collection, analysis and interpretation, assisted in drafting and revised the manuscript. GO performed data collection, data review and interpretation, and revised the manuscript. CP designed the study, performed data review and interpretation, and revised the manuscript. PV performed data collection and revised the manuscript. MVH performed the statistical analysis. SAM designed the study and data analysis, performed data review and interpretation, drafted and revised the manuscript. All authors have read and approved the final manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the Henry Ford Hospital Institutional Review Board.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Viarasilpa, T., Panyavachiraporn, N., Osman, G. et al. Electrographic Seizures in Patients with Acute Encephalitis. Neurocrit Care 30, 207–215 (2019). https://doi.org/10.1007/s12028-018-0599-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0599-4