Abstract
Background
Children presenting to the emergency department with acute psychosis or hallucinations sometimes undergo a head CT to evaluate for a causative lesion. The diagnostic yield of head CT in this scenario has not been reported.
Objective
To determine the yield for head CT in children with acute psychosis or hallucinations.
Materials and methods
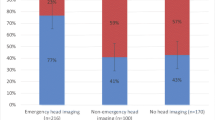
We retrospectively searched the radiology report database over a 7.5-year period for head CT reports for pediatric emergency department patients using the following keywords: hallucination, psychosis, psychotic or “hearing voices.” All reports were categorized as normal or abnormal, and we reviewed and categorized the abnormal cases. We calculated the 95% confidence interval for abnormal CTs using the method of Clopper and Pearson.
Results
We identified 397 pediatric emergency department head CTs. We excluded one non-diagnostic exam. We excluded 34 additional cases (which were all normal) because of clinical indications that might have independently triggered a head CT. Of the remaining 362 cases, 12 reports described abnormalities or variants and we reviewed them individually. Based on consensus review, four were normal, four had congenital malformations, three had encephalomalacia versus demyelination and one demonstrated cortical atrophy. There were no cases with actionable findings such as mass, hemorrhage, infection or hydrocephalus. The 95% confidence interval for a CT demonstrating causative findings was calculated at 0–0.82%.
Conclusion
In the absence of concerning factors such as focal neurological deficits, evidence of central nervous system infection, trauma or headache, routine screening head CT might not be warranted in children presenting with acute psychosis or hallucinations.


Similar content being viewed by others
References
Donofrio JJ, Santillanes G, McCammack BD et al (2014) Clinical utility of screening laboratory tests in pediatric psychiatric patients presenting to the emergency department for medical clearance. Ann Emerg Med 63:666–675.e3
Clopper CJ, Pearson ES (1934) The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 26:404–413
Hollister LE, Boutros N (1991) Clinical use of CT and MR scans in psychiatric patients. J Psychiatry Neurosci 16:194–198
Alciati A, Fusi A, D'Arminio Monforte A et al (2001) New-onset delusions and hallucinations in patients infected with HIV. J Psychiatry Neurosci 26:229–234
Maruca-Sullivan PE, Goldenberg MN, Cone DC, Ciarleglio J (2016) Missing the point: self-inflicted traumatic brain injury in psychosis. BMJ Case Rep https://doi.org/10.1136/bcr-2016-216767
Coentre R, Silva-Dos-Santos A, Talina MC (2016) Retrospective study on structural neuroimaging in first-episode psychosis. Peer J 4:e2069
Williams SR, Koyanagi CY, Hishinuma ES (2014) On the usefulness of structural brain imaging for young first episode inpatients with psychosis. Psychiatry Res 224:104–106
Larson EB, Mack LA, Watts B, Cromwell LD (1981) Computed tomography in patients with psychiatric illnesses: advantage of a "rule-in" approach. Ann Intern Med 95:360–364
Ananth J, Gamal R, Miller M et al (1993) Is the routine CT head scan justified for psychiatric patients? A prospective study. J Psychiatry Neurosci 18:69–73
Bain BK (1998) CT scans of first-break psychotic patients in good general health. Psychiatr Serv 49:234–235
Maurice-Williams RS, Dunwoody G (1988) Late diagnosis of frontal meningiomas presenting with psychiatric symptoms. Br Med J 296:1785–1786
Bunevicius A, Deltuva VP, Deltuviene D et al (2008) Brain lesions manifesting as psychiatric disorders: eight cases. CNS Spectr 13:950–958
National Institute for Health and Care Excellence (2008) Structural neuroimaging in first-episode psychosis. https://www.nice.org.uk/guidance/ta136. Accessed 7 Aug 2018
Lesher AP, Myers TJ, Tecklenburg F, Streck CJ (2010) Anti-N-methyl-D-aspartate receptor encephalitis associated with an ovarian teratoma in an adolescent female. J Pediatr Surg 45:1550–1553
Kvícala V, Vymazal J, Nevsimalová S (1983) Computed tomography of Wilson disease. AJNR Am J Neuroradiol 4:429–430
Schörner W, Meencke HJ, Felix R (1987) Temporal-lobe epilepsy: comparison of CT and MR imaging. AJR Am J Roentgenol 149:1231–1239
Reddy MSS, Thippeswamy H, Ganjekar S et al (2018) Anti-NMDA receptor encephalitis presenting as postpartum psychosis — a clinical description and review. Arch Womens Ment Health 21:465–469
Kim TJ, Kim IO, Kim WS et al (2006) MR imaging of the brain in Wilson disease of childhood: findings before and after treatment with clinical correlation. AJNR Am J Neuroradiol 27:1373–1378
Swinburne NC, Bansal AG, Aggarwal A, Doshi AH (2017) Neuroimaging in central nervous system infections. Curr Neurol Neurosci Rep 17:49
Ng P, McGowan M, Goldstein M et al (2018) The impact of CT head scans on ED management and length of stay in bizarre behavior patients. Am J Emerg Med 36:213–217
Nadler A, Avner D, Khine H et al (2018) Rising clinical burden of psychiatric visits on the pediatric emergency department. Pediatr Emerg Care https://doi.org/10.1097/PEC.0000000000001473
Trofimova A, Vey BL, Mullins ME et al (2018) Imaging of children with nontraumatic headaches. AJR Am J Roentgenol 210:8–17
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Cunqueiro, A., Durango, A., Fein, D.M. et al. Diagnostic yield of head CT in pediatric emergency department patients with acute psychosis or hallucinations. Pediatr Radiol 49, 240–244 (2019). https://doi.org/10.1007/s00247-018-4265-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4265-y