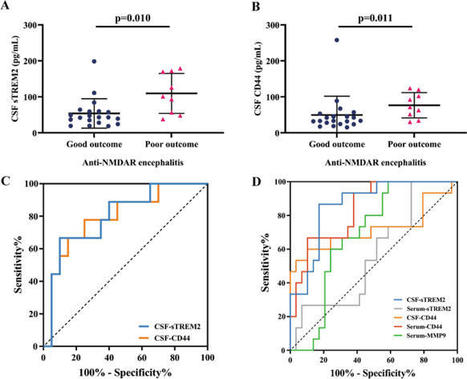
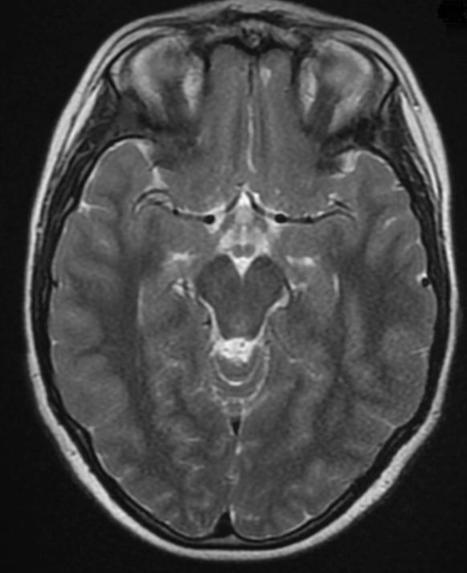
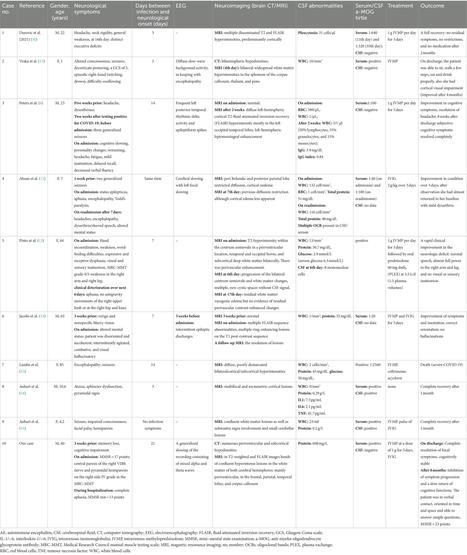
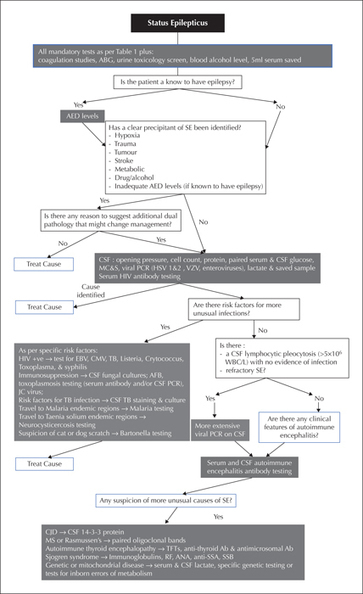
Figures Tables Table 1 Table 2 The diagnosis and management of epilepsy, including first seizures and status epilepticus, depends largely on thorough history taking, including a forensic approach to obtaining witness accounts and information about the background and circumstances affecting an individual. Investigations, such as EEG and MRI, as will be covered in separate articles in this series, and are of particular value in identifying the type of epilepsy and underlying cause, and contributing to predicting risk of recurrence after a first unprovoked seizure. However, at least 55% of new-onset seizures (Beghi et al., 2010), including around 50% of status epilepticus cases, are provoked (acute symptomatic seizures). In patients with known epilepsy, systemic illnesses may also contribute to deterioration in seizure control. It is in this context that laboratory (blood, urine, cerebrospinal fluid) investigations are especially important. This review summarises the role of laboratory investigations in the diagnosis and management of people presenting with seizures, to provide an educational resource to help the managing clinician decide which patients should receive laboratory tests and which types of tests should be ordered. This is a core competency (Level 1) defined in the ILAE Epileptology Curriculum (Blümcke et al., 2019), which is relevant for all health professionals involved in the diagnosis and management of people with epilepsy. FIRST SEIZURE Although not key to the diagnosis of a first seizure, or new-onset seizures, some laboratory investigations performed as soon as possible after the seizure onset can be key to identifying the cause, specifically with respect to determining if the event is provoked (acute symptomatic) or unprovoked. Acute symptomatic seizures occur at the time of, or in close association with, a documented brain insult (Thurman et al., 2011), which likely account for over 50% of all first seizures (Hauser and Beghi, 2008). Importantly, with an acute symptomatic seizure, the key priority in management is addressing the cause. Some untreated are rapidly fatal, but if successfully managed, are associated with full recovery and a recurrence risk of less than 3% (Pohlmann-Eden et al., 2006). In contrast, the five-year risk of recurrence is at least 10-fold higher following a first unprovoked seizure (Marson et al., 2005). Thus, correctly distinguishing between provoked and unprovoked at the outset has important implications for the individual both in the first few hours and also with respect to longer-term management and safety advice including driving. Almost any acute brain insult, including stroke and trauma, can result in an acute symptomatic seizure, but in the context of this article, the most important triggers are metabolic, toxic, infectious and inflammatory. Metabolic: Metabolic derangements causing seizures can be extremely dangerous and need to be treated urgently, therefore checking (capillary and then serum) glucose, sodium, calcium and magnesium and renal and liver function should be done as soon as possible. These, and other essential initial tests, are summarized in table 1. The only exception is children with simple febrile seizures, for which there is consensus that additional investigations are not required unless there are other clinical markers of concern (American Academy of Pediatrics, 2011; Wilmshurst et al., 2015). Glucose: In patients of any age, including neonates for whom it is especially important (Gataullina et al., 2015), checking that the blood glucose is within normal range should be of the utmost priority, as untreated hypoglycaemia can rapidly lead to irreversible neurological damage and death. In adults, a glucose level below 2 mM/L or above 25 mM/L is usually required to produce seizures, the latter most commonly in older patients with type II diabetes, whereas hyperglycaemia accompanied by ketosis is not usually epileptogenic (Nass et al., 2017; Ohara et al., 2017). Additionally, diabetes mellitus is an independent risk factor for seizures in the elderly, therefore HbA1c (glycosylated haemoglobin) testing should be performed in older patients as a measure of longer-term blood glucose (Baviera et al., 2017). Sodium: Hyponatraemia is the commonest electrolyte disturbance to provoke seizures in adults. The mechanism for this is cerebral oedema, which is due to the osmotic gradient between the plasma and the brain. The more rapid the fall in sodium, the fewer adaptive responses the brain can produce to protect itself and more severe the resulting cerebral oedema will be. Whilst less common, children are particularly vulnerable to the effects of cerebral oedema as they have relatively large brains compared to their scull size (Nardone et al., 2016). Correction of low sodium must be carefully monitored to avoid the potentially devastating complication of pontine myelinolysis. Hypernatraemia is a much less common cause of seizures but may produce them due to brain shrinkage (Castilla-Guerra et al., 2006). Calcium and magnesium: Hypocalcaemia, and less frequently hypercalcaemia, can provoke seizures. When this is identified, further investigations as to the cause, usually in consultation with an endocrinologist, may also be required, which is beyond the scope of this article. Hypomagnesaemia is much less common but can cause seizures in any age group. Potassium: Derangements in serum potassium are clearly very dangerous from a cardiovascular and neuromuscular perspective, and so important to identify, but do not cause central nervous system (CNS) symptoms or seizures (Riggs, 2002; Castilla-Guerra et al., 2006). Urea, nitrogen and creatinine: Seizures are common in patients with renal failure due to elevated urea. It should be noted that non-convulsive status and status epilepticus may mimic uremic encephalopathy, therefore it is particularly important to consider these as possible diagnoses in renal patients (Titoff et al., 2019). Infective and inflammatory disease: Infective or inflammatory causes should be considered in any one with a history of fever or recent malaise, and untreated can prove fatal. Febrile seizures are particularly common in children up to school age, but seizures can be the presenting feature of infection or inflammatory conditions at any age. All patients should have a full blood count (FBC) and test for C-reactive protein (CRP) as a minimum. Mild leucocytosis and raised CRP are commonly found postictally due to a generalised inflammatory response, with a lack of evidence to define clear levels above which a more aggressive search for infection should follow. Further investigations will depend on the clinical history, examination, observations and sometimes repeated laboratory tests to look for trends. If there are clinical reasons to suspect a central nervous system infection or sepsis (which can itself be associated with an encephalopathy), blood and urine cultures, and cerebrospinal fluid (CSF) samples should be obtained. In any patient with focal signs or who has not completely recovered, brain imaging (typically brain CT) will be needed before CSF can be collected (indications for brain imaging in epilepsy are covered in a separate article). CSF opening pressure should be recorded (for example, venous sinus thrombosis can present with seizures and a high opening pressure), and CSF sent for routine tests including cell count, protein, sugar (with matched blood sugar), bacterial culture and viral PCR. Depending on the clinical history and examination, additional tests for fungal or mycobacterial infections, and oligoclonal bands, might also be appropriate. It is sensible to take more than required for initial tests, with a saved sample for additional tests, should they be required based on initial results, or other information that emerges later. In persons presenting with behavioural changes, memory problems, a high frequency of new-onset seizures or (as will be covered later) status epilepticus, if other tests have been non-contributory, the possibility of an autoimmune encephalitis needs to be considered. This should be investigated alongside specific serum and CSF antigens (Dalmau and Graus, 2018). If there is any suspicion of multiple sclerosis, then oligoclonal bands may also be important. Clinical treatment decisions usually have to be made before the results of these additional investigations are available (this can take 2-3 weeks, even in well-resourced settings), further discussion of which is beyond the scope of this article, but decision-making algorithms have been created to aid this (Graus et al., 2016; Wagner et al., 2018). Intoxication: In parallel with assessing for metabolic and infectious causes of a first seizure, one should consider whether recreational drugs, alcohol or medications may have been precipitants. It is not possible to provide absolute cut-off thresholds for these, as inter-individual differences in seizure susceptibility play a substantial role (Brathen et al., 2005), but the detection of substances at all in the appropriate time window may be highly relevant. Importantly, when drug or alcohol-provoked seizures are identified, co-morbid epilepsy, sometimes as yet undiagnosed, is not uncommon and the recurrence risk (due to recurrent ingestion or epilepsy) is also higher, therefore additional investigations as for any first unprovoked seizure (EEG and MRI) should still be undertaken at a later date. Alcohol: Alcohol withdrawal, particularly in combination with sleep deprivation, is a very common cause of seizures. Seizures usually occur 6-48 hours after cessation of drinking (Leach et al., 2012). As markers of chronic alcohol consumption, mean corpuscular volume (MCV) and serum gamma glutamyl transferase (GGT) may be useful, although the latter may be elevated due the ingestion of certain drugs, including many antiepileptic drugs (AEDs). Benzodiazepines and recreational drugs: A broad range of widely available, though mostly illegal, stimulant drugs can cause seizures even at low levels of consumption. Cocaine, crack, normeperidine, meperidine, methaqualone, glutarimide, ethylenedioxymethamphetamine and a range of other synthetic stimulants are considered high risk, along with phencyclidine and quatadine (Beghi et al., 2010). Other drugs with narcotic effects, such as benzodiazepines, synthetic cannabinoids, gamma-hydroxybutyrate and opiates including heroin, may trigger seizures during their withdrawal (Leach et al., 2012). The use of multiple intoxicants is common, so rather than testing for individual agents, urinary drug screening for metabolites is recommended in the first instance. Prescription medications: Drugs such as antibiotics, antidepressants and antipsychotics in routine use rarely induce seizures, even in people with epilepsy other than in the context of significant overdoses. Usually patient history is sufficient, but to identify intoxication or slow metabolizers, serum drug monitoring may be useful. Was it a seizure? Diagnostic uncertainty. A number of laboratory investigations have also been proposed as potentially useful where there is diagnostic uncertainty as to the nature of an event, specifically to discriminate between epileptic seizures, psychogenic non-epileptic seizures (PNES) and syncope. However, whilst of academic interest, none should be considered diagnostic and, in most instances, will not be useful. Many of these markers are only raised in tonic-clonic seizures, and even then, they are not wholly reliable as summarized below. Clinical history and witness accounts remain the mainstay in the diagnosis of epileptic seizures. Prolactin is the most widely suggested but has substantial limitations: It is only useful when there is a known (pre-event) baseline and taken 20 minutes post-event, which is rarely achievable. It does not always rise after an epileptic seizure; it may rise due to other events such as syncope and its levels depend on many other variables including age, gender, circadian rhythm, medications, pregnancy and even psychological stress. In status epilepticus, prolactin levels may normalise after an initial rise (Abubakr and Wambacq, 2016; Nass et al., 2017). Creatinine kinase (CK): A transitory (sometimes very substantial) increase in creatinine kinase, 24-72 hours after a tonic-clonic seizure (TCS), is a relatively specific but not sensitive marker (i.e. raised CK points towards a TCS, but a normal CK does not rule it out). However, it should be noted that CK may be elevated due to other conditions such as a post-syncopal long lie. Nevertheless, a raised CK is important to help identify patients who will be at higher risk of developing acute kidney injury as a result of muscle breakdown due to seizures, and these patients will need careful monitoring and treatment if this develops (Nass et al., 2017). Ammonia: A transitory increase in ammonia, lasting 3-8 hours after an event, is a relatively specific but not sensitive marker of a convulsion. Patients with cirrhosis and no history of convulsions will have persistently elevated ammonia. Valproic acid may also cause elevations in serum ammonia (Nass et al., 2017). Lactate: A raised lactate level above 2.45 mmol/L, taken within two hours of the event, has been postulated to be a useful indicator of a likely TCS. However, this is not very sensitive (Matz et al., 2016). Furthermore, simulated seizures can also produce markedly raised lactate levels (Lou Isenberg et al., 2020). There are also numerous other causes of a raised lactate level, such as sepsis, tumour or liver disease, therefore this cannot be considered diagnostic in isolation. Other parameters in infants: In infants (under one year) with new-onset seizures (also covered below), ideally, the genetic syndrome of pyridoxine-deficiency epilepsy should be excluded (van Karnebeek et al., 2016) based on determination of alpha-aminoadipic semialdehyde/pyrroline 6’ carboxylate (in urine, plasma or cerebrospinal fluid) and ALDH7A1 molecular analysis. STATUS EPILEPTICUS In the previous sections we discuss what to test the first time someone presents with seizures, and the limited utility of laboratory testing in the case of diagnostic uncertainty. In this section, we discuss what laboratory tests to perform in the patient who does not stop seizing, i.e. presents with status epilepticus (SE). As with any seizure, the diagnosis of status epilepticus is primarily a clinical one, supported, when possible, by neurophysiological (EEG) data (Trinka et al., 2015). The role of laboratory testing is, as with first seizures, to identify the cause but also, particularly in convulsive SE, to evaluate the possible consequences of what is a life-threatening medical emergency, to inform on ongoing management. A suggested approach to laboratory testing for SE is summarized in figure 1. For all patients: All patients in SE should have the mandatory blood tests described in table 1. In addition, coagulation studies and creatine kinase, an arterial blood gas and toxicology screening should be performed. This is to establish a baseline, as part of investigating the cause, and to identify those who might be at particularly high risk of complications, such as those with acute kidney injury (from rhabdomyolysis) or a coagulopathy. Patients with known epilepsy: An antiepileptic drug (AED) level must be checked as low AED levels are the most common cause of SE in this group of patients (Trinka et al., 2012). Ideally, AED levels should be tested on a sample taken prior to any AED administration. In practice, as relevant background information may not be available at the point of presentation, it is sensible to take an additional 5 mL of serum saved for future testing at the outset, before AEDs given as part of treating the episode confound interpretation. Specific AED levels can then be requested for the original sample at a later date when prescribed drugs are known. AED levels are most useful/reliable if a prescribed drug is not-detected, indicating poor adherence, though beyond that the results should be interpreted with caution, ideally compared to the individual's own therapeutic concentration as this may vary from the standard reference ranges (Lunardi et al., 2019). Therapeutic drug monitoring is not routinely recommended during SE treatment as AED concentrations may actually exceed the published target concentrations (NICE, 2012 [Update 2019]), other than in refractory or super-refractory cases in which confirming at least adequate levels before an agent is considered ineffective can be useful. Infectious disease: Lumbar puncture should be performed in any patient with a suspicion of CNS infection or inflammation or in any patient without another clear cause of SE. A CSF pleocytosis of greater than 5 × 106/L is not usually caused by SE alone, and so this should prompt careful investigation of any infectious or inflammatory cause (Frank et al., 2012; Scramstad and Jackson, 2017; Johnson et al., 2014). Testing for HIV is also important to consider if not already known. Common infectious causes of SE are bacterial (e.g. meningococcus, pneumococcus and haemophilus), viral (e.g. herpes simplex 1 and enteroviruses) or protozoal (Lowenstein et al., 2014; He et al., 2016). There is considerable regional variation in likely infectious causes of SE, for example Japanese encephalitis is endemic in South-East Asia, malaria in sub-Saharan Africa and Asia, and neurocystericosis in Latin America, India and Africa, therefore the country of origin and travel history will impact on choice of laboratory investigations. HIV-positive patients will need a more comprehensive workup to exclude opportunistic infections (Solomon et al., 2012). Immunological & inflammatory disease: Autoimmune encephalitis (AE) is an uncommon but potentially treatable cause of SE. Identifying it is of vital importance because it may be associated with AED-refractory seizures that will only improve with immunotherapy or, in the case of paraneoplastic encephalitis, with treatment of the underlying cancer. Our knowledge of the autoimmune encephalitides and the antibodies associated with them is relatively recent and continues to evolve (Dalmau and Graus, 2018). Multiple anti-neuronal antibodies may be implicated, including, likely, some yet to be discovered, with a range of presentations. Those most frequently associated with seizures and status epilepticus include: antibodies against the GluN1 subunit of the NMDA (N-methyl-D-aspartate) receptor and anti-GAD, anti-GABA (gammaaminobutyric acid) type A and B receptor, anti-LGI1 receptor (leucine-rich glioma inactivated 1), and anti-Hu antibodies (Jacobs et al., 2003; Johnson et al., 2010; Lancaster et al., 2010; Illingworth et al., 2011; Suleiman et al., 2011; Bien, 2013; Petit-Pedrol et al., 2014). Any patient with a history of new-onset cognitive or memory deficits, speech problems, movement disorder or behavioural changes leading up to the SE, when no other obvious cause is identified, should be investigated for autoimmune encephalitis. In practice, rather than requesting full panels for all patients, discussion with the local laboratory, to agree priorities and understand local techniques and their sensitivity and specificity which can vary, is recommended. Anti-GAD (glutamic acid decarboxylase) antibodies are also not uncommonly identified, but also found in a range of other disorders including diabetes, and of uncertain pathogenicity (Alexopoulos and Dalakas, 2013). CSF will usually show a mild pleocytosis, but it may be normal. Both serum and CSF should be tested for antibodies (Graus et al., 2016). For further guidance on when to investigate for AE, see figure 1. A diagnosis of Hashimoto's encephalopathy may be considered in patients who have no anti-neuronal antibodies in serum and CSF. These patients should be investigated with thyroid function tests, and serum thyroid peroxidase and thyroglobulin antibodies, in order to assess if they meet the diagnostic criteria. In patients who are negative for anti-neuronal antibodies, and do not meet the criteria for Hashimoto's encephalopathy, further antibody testing in research laboratories for new antibodies may be considered, and the patient may be evaluated for the diagnosis of auto-antibody-negative but probable autoimmune encephalitis (Graus et al., 2016). Systemic autoimmune conditions may also cause SE, including Sjogren's and systemic lupus erythematosus, and serum autoantibody testing may be useful in these cases. SE can also occur in the context of multiple sclerosis and Rasmussen's encephalitis, but almost never as the presenting symptom. If there is clinical suspicion of either of these inflammatory conditions, then testing of serum and CSF oligoclonal bands may be supportive in diagnosis. Cryptogenic new-onset refractory status epilepticus (NORSE) and what may be a subtype of the same condition, febrile infection-related epilepsy syndrome (FIRES), are characterised by the rapidly progressive onset of seizures and encephalopathy that evolve into prolonged super-refractory SE over a few days. In the case of FIRES, this is preceded by a minor febrile infection (Gaspard et al., 2018). Both are thought to have an inflammatory/autoimmune basis, possibly involving a post-infection cytokine-medicated mechanism. There are currently no diagnostic laboratory tests for these conditions. Genetic, mitochondrial and other disorders: There are a number of mitochondrial diseases which, though rare, have SE as a prominent feature. These include: Alpers disease; mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes (MELAS); Leigh syndrome; and myoclonic encephalopathy with ragged red fibres (MERRF) (Trinka et al., 2012; Myers et al., 2019). For these patients’ serum and CSF, testing for lactate is recommended, though alone, this neither proves nor excludes a mitochondrial disorder, and where there is a strong clinical suspicion, specialist advice should be sought. Inborn errors of metabolism, such as porphyria, Wilson's disease and Alexander's disease, as well as chromosomal aberrations such as Angelman syndrome, may be investigated with specific genetic and/or laboratory testing. A comprehensive list of all the genetic and mitochondrial disorders which may cause SE is beyond the scope of this article, but covered in Myers et al (2019). ROLE OF BLOOD TESTS IN LONG-TERM MONITORING Some authorities suggest laboratory tests should ideally be performed prior to initiation of, and during treatment with, almost any AED (Patsalos and St. Louis, 2018). In most instances, some baseline parameters will nevertheless be available as part of an initial investigation of the presenting seizure or associated illness. Beyond that, the only other recommended pre-treatment test (table 2) is when treatment with carbamazepine, oxcarbazepine or eslicarbazepine is considered in individuals of Southeast Asian descent. The human leucocyte antigen (HLA) allele, HLA-B*1502, is highly prevalent in this population (up to 15% in Hong Kong, Thailand and the Philippines), and strongly associated with severe cutaneous hypersensitivity reactions (Stevens Johnson syndrome, toxic epidermal necrolysis). For carbamazepine, hetero- or homozygosity is estimated to show 98.3% sensitivity and 97% specificity for the development of SJS/TEN, with a 100% negative predictive value. Guidelines for screening prior to treatment are now in place in several developed countries (Fowler et al., 2019), though simply avoiding these drugs when alternatives are readily available is also of course entirely appropriate. A number of other alleles have also been identified, but none with such a strong association. According to most practitioners and guidelines, regular (e.g. annually or more) blood test monitoring of children or adults with epilepsy is not recommended as routine and should only be performed if clinically indicated (NICE, 2012 [Update 2019]). Infrequent monitoring, e.g. at 2-5-year intervals, is almost certainly sufficient. That said, awareness of the more common potential laboratory abnormalities associated with AED use is important. Patients need to be advised to seek medical advice if indicative symptoms occur, and non-specialists need to know which specific abnormalities to test for depending on the AED in question, and the clinical situation. It is similarly just as important to know what minor derangements can be safely attributed to AED use, without needing any change in treatment or further investigation. Broad recommendations by drug are summarized in table 2. Haematologic reactions: Many AEDs are associated with a spectrum of haematological side effects. These include aplastic anaemia (carbamazepine, valproate and phenytoin), megaloblastic anaemia (phenytoin, phenobarbital and primidone) and thrombocytopaenia (carbamazepine and valproate). Transient leukopaenia and neutropaenia may also occur, especially in patients with low pre-treatment levels. Clinical indications to test include the development of a sore throat/bacterial infection within a few weeks of starting or a dose increase, new bleeding or bruising, or excessive fatigue. Second and third-generation AEDs tend to be associated with fewer haematological side effects, but for newer drugs, it must not be forgotten that rare but potentially dangerous effects can sometimes only become apparent some years after licensing. For all AED therapy, discontinuation is usually not indicated, unless symptoms are severe. In general, withdrawal should be considered if cell count falls below: 2,000/mL for white blood cells, 1,000/mL for neutrophils, 3.5 × 106/mL for red blood cells (11 g/dL for haemoglobin concentration) and 80,000/mL for platelets (Verrotti et al., 2014). Overwhelmingly, haematological reactions are reversible after withdrawal and do not need any special treatment (Callaghan et al., 1985). Electrolytes and pH changes: Hyponatremia is a common finding with carbamazepine, oxcarbazepine and eslicarbazepine treatment, most likely due to antidiuretic effects. It is usually mild (>130 mmol/L) and asymptomatic, though often causes undue concern if picked up incidentally. Concurrent use of other agents, such as antihypertensives and serotonin re-uptake inhibitors, increases the risk. Levels between 125 and 130 nmol/L (moderate), particularly when chronic, may also appear to be asymptomatic, though can also be associated with subtle symptoms and increased morbidity and mortality in some contexts. Symptoms, when present, range from minor unsteadiness, falls, and reduced concentration through to confusion, nausea, and in severe cases, life-threatening cardiorespiratory distress or coma (Williams et al., 2016). Thorough clinical assessment is essential, with management of symptoms (or lack of) being a more important factor than absolute sodium. Additional investigations (including plasma and urine osmolality) are indicated in all but the mildest cases to exclude and address other contributors and inform decisions about the suspect AED. Asymptomatic metabolic (renal tubular) acidosis is common during topiramate treatment (Garris and Oles, 2005), and also seen with other carbonic anhydrase inhibitors, zonisamide (Baulac et al., 2014) and acetazolamide (Hamed, 2017). In some, this is likely associated with an increased the risk of nephrolithiasis (Kuo et al., 2002; Hamed, 2017) and a crystalline nephropathy, although not all studies support this (Shen et al., 2015). Hepatotoxicity: Use of many AEDs, especially older drugs such as phenytoin, carbamazepine and valproate (Bjornsson, 2008; Hamed, 2017), as well as some of the newer agents including cannabidiol, is associated with abnormalities of liver function. Mild derangements based on liver function tests (<double the normal upper limit of normal) are usually not of concern unless symptomatic or deteriorating on repeat testing. Valproate use also causes raised ammonia levels, sometimes causing a reversible encephalopathy (Chopra et al., 2012), though, of note, a non-hyperammonaemic valproate encephalopathy is also recognized. Testing should be considered in any patient presenting with confusion, lethargy or drowsiness after initiation or a dose increase. Bone health: An increased risk of fracture related to AED use is now well established (Theochari and Cock, 2018). Whilst a broad range of parameters such as markers of bone turnover have been evaluated in research studies, the only laboratory measure independently associated with fracture risk is vitamin D. AED use and epilepsy are both risk factors for hypovitaminosis D, with likely pharmacological and other contributors (e.g. reduced sunlight exposure, lower physical activity). Current evidence supports testing serum vitamin D, calcium, albumin and alkaline phosphatase (“bone profile”), 2-5 times yearly in adults and children on AEDs (NICE, 2012 [Update 2019]), with vitamin D supplementation as required, aiming for a yearly average serum level of >50nmol/L (Dobson et al., 2018). Most of the evidence relates to enzymes inducing older AEDs, specifically carbamazepine, phenytoin and barbiturates, in whom more frequent monitoring (e.g. annually) may be justified (Arora et al., 2016). However, there is no doubt that valproate (and enzyme inhibitor) is also implicated (MHRA, 2009), and the paucity of evidence against newer AEDs may just reflect less cumulative exposure and should not be considered to indicate a lack of risk. It is reasonable to assume, unless proven otherwise, that other enzyme inducers carry at least similar risks, and other AEDs may carry some risk, though some reassuring data with respect to lamotrigine and levetiracetam is emerging (Theochari and Cock, 2018). Cardiovascular risk factors; Obesity, diabetes and hypercholesterolaemia are all independently associated with cardiovascular disease and premature mortality. These risks apply as much to people with epilepsy as to others in the population. Several antiepileptic drugs can be associated with weight gain, in particular, valproate, pregabalin, gabapentin, and vigabatrin, in whom monitoring of lipid profile and glucose may be appropriate and inform lifestyle change, or in some instances, a change in AED. In recent years, interest in the potential for AEDs to influence other circulatory markers of vascular risk, such as homocysteine, folate, C-reactive protein, and more recently, homoarginine and asymmetric dimethylarginine, has also emerged (Kim et al., 2013; Sarecka-Hujar et al., 2019). However, the clinical implications of this in practice remain uncertain, with insufficient evidence as yet to guide a monitoring or intervention strategy. Therapeutic drug monitoring: Therapeutic drug monitoring (TDM) is a tool which, correctly utilized, can be extremely helpful in optimizing treatment for some individuals. Certainly for many drugs, there is a better correlation between serum levels and efficacy than with the oral dose (Patsalos et al., 2018). However, for the vast majority of patients, if they are free of seizures and side effects, Class I evidence now supports that knowing the serum level is of little, if any, benefit in routine practice (Aícua-Rapún et al., 2020). Thus, taking costs into account, routine monitoring is generally not recommended (NICE, 2012 [Update 2019]). TDM can, however, be critical to support (or refute) a suspicion of non-adherence or for suspected toxicity or seizure persistence despite prescribing of an adequate dose (to identify fast metabolisers or non-compliance), when a formulation change is to occur and when pharmacokinetic variability is expected (e.g. in children or the elderly, pregnancy, or for hepatic or renal disease), or drug interactions are anticipated (Patsalos et al., 2018). This is particularly so with phenytoin (which exhibits saturation kinetics, meaning even a small change in dose or metabolism can result in substantial changes in level), and in situations where reliance on clinical judgement alone is felt to be insufficient, for example, when even a single, potentially preventable seizure, after a period of remission, might have significant consequences. In this situation, if available, the best comparator is the “individual therapeutic concentration”, i.e. a plasma AED concentration trough level taken during a time of optimum therapeutic response on an established dose. Individualized therapeutic AED monitoring is accepted as much more meaningful than a comparison to fixed reference ranges (Patsalos et al., 2018). Strictly speaking, predicting drug adherence or non-adherence based on AED plasma levels is only possible when the level is compared to that individual's therapeutic concentration (Lunardi et al., 2019), though in practice reasonable inferences can be drawn from big fluctuations or undetectable levels despite stable prescribed doses. KNOWN EPILEPSY WITH DETERIORATION OF CONTROL A frequent clinical challenge is represented by people with established epilepsy presenting to acute medical services, reporting a deterioration in seizure control. This might be a single unprovoked seizure after a period of remission, a reported increase in seizure frequency, or seizure clusters sometimes escalating and leading to concern about imminent status epilepticus. In this situation, it is important to remember that all the factors discussed earlier that can trigger acute symptomatic seizures, or status epilepticus, can similarly influence seizure frequency in individuals with established epilepsy, therefore a similar approach to laboratory testing is recommended. Excluding intercurrent infection, as well as checking AED levels and alcohol and toxicology screens can be key, yet the latter in our experience are often overlooked in favour of CT or even EEG, which are rarely informative or indicated in this context. PREGNANCY IN WOMEN WITH EPILEPSY Specific issues pertain to women with epilepsy who might become or who are pregnant: Some AEDs are known to have teratogenic effects and so choice and optimization of drug treatment in advance of any potential pregnancy in women of childbearing age is particularly important (Tomson et al., 2019). Non-adherence rates are increased during pregnancy (likely due to concerns over teratogenicity as well as other factors such as vomiting) (Schmidt et al., 1983). Therefore, pre-pregnancy counselling regarding the importance of treatment continuation, because of the maternal and foetal risks of uncontrolled seizures, is extremely important (Pennell, 2003). Serum levels of most AEDs fall during pregnancy due to haemodilution, changes in absorption and metabolism and increased excretion. Whilst the seizure frequency of most women will remain unchanged or fall during pregnancy, a significant number of them will experience an increase in seizures, likely due to medication non-compliance and reduced serum levels (Harden et al., 2009; Pennell, 2003). In light of the above issues, the question arises as to the utility of therapeutic drug monitoring (TDM) during pregnancy, and to some, identifying a pre-pregnancy individual therapeutic concentration and then monitoring and adjusting the dose during pregnancy may seem like an obvious strategy. However, in the only study to date to formally address this in a prospective and blinded manner, there was no evidence to support “treating the level” over and above standard practice (increasing the dose in response to changes in seizure frequency) (Thangaratinam et al., 2018). An exception to this might be lamotrigine which exhibits markedly increased clearance during pregnancy, resulting in a reduction of plasma levels of around 65% in the second and third trimester (Petrenaite et al., 2005). There is some evidence that TDM of lamotrigine during pregnancy may be superior to clinical monitoring alone in reducing seizure deterioration (Pennell, 2003; Pirie et al., 2014). Both the ILAE and the American Academy of Neurology currently recommend TDM during pregnancy in women on an AED known to undergo substantial clearance changes, including lamotrigine, levetiracetam, oxcarbazepine and phenytoin. When a pre-pregnancy level is unknown, increasing the dose, at least in women with a history of tonic-clonic seizures, should be considered in any case (Tomson et al., 2019). When AED doses have been increased during pregnancy, tapering after delivery will usually be required. TDM may also be useful if there is concern about toxicity during this time, although in practice the decision will usually be made on clinical grounds before any level is available. The other important test to do in relation to pregnancy is ensuring adequate vitamin D status ideally before conception, but also during pregnancy. Vitamin D is essential for foetal development, therefore checking 25-hydroxyvitamin D levels at least once early on, and supplementing accordingly, is recommended (Hart et al., 2015, Roth et al., 2017). Folate supplementation (all, at least 0.4 mg/day) is also recommended but does not require serum monitoring. Similarly, there is no requirement for monitoring vitamin K or clotting parameters in women, including those on enzyme-inducing AEDs. Oral or intramuscular vitamin K administration in neonates is standard care for all women in many countries, and there is no evidence that the historical practice of additionally supplementing the mother during the last trimester is necessary (Sveberg et al., 2015; Panchaud et al., 2018). OTHER CONSIDERATIONS IN RARE OR UNUSUAL CASES A range of rare but important neurometabolic disorders can cause epilepsy (Lee et al., 2018), the detailed discussion of which is beyond the scope of this article and will almost always require specialist assessment in a tertiary centre. Some are particularly important not to miss, as AEDs will often be ineffective, whereas targeted therapy for the underlying disorder, in the form of supplements or dietary modifications, can substantially improve outcomes. Glutamine transporter type 1 deficiency syndrome (Glut1DS): This classically presents in infancy with seizures that are treatment-resistant or influenced by fasting, associated with developmental delay, acquired microcephaly and a range of movement disorders. However, a much broader phenotype, including later onset and paroxysmal movement disorders, is also now recognized (De Giorgis and Veggiotti, 2013). Glut1 facilitates glucose transport across the blood-brain barrier and the initial diagnostic step, feasible worldwide, is a fasting lumbar puncture which will show relatively low CSF glucose (hypoglycorrhachia) compared to blood glucose and a low-to-normal lactate level. Genetic confirmation by analysis of the solute carrier family 2 (facilitated glucose transporter) member 1 (SLC2A1)gene may then be performed. Early diagnosis is critical because it allows prompt initiation of treatment with a ketogenic diet (Klepper and Leiendecker, 2007; De Giorgis and Veggiotti, 2013). Vitamin B6-dependent epilepsies: The B6 vitamins, in particular pyridoxal-5’-phophate (PLP), are involved in over 70 human pathways, including amino acid and neurotransmitter metabolism (Wilson et al., 2019). In any neonate or infant presenting with AED-resistant seizures, often myoclonic in the first days of life, plasma, urine and ideally CSF samples should be collected and frozen at -80̊C for biomarkers. Hypoglycaemia and lactic acidosis may be present in the acute phase, but testing should not delay a prompt empirical trial of treatment with pyridoxine in the first instance, with next steps dependent on response. Later-onset cases, including status epilepticus in adults, have also been reported but appear to be extremely rare. Mitochondrial disorders are another important group, characteristically causing a combination of different types of focal seizures and can pose a significant risk of SE (Bindoff and Engelsen, 2012). Indicators to consider onward referral include seizures developing in association with failure to thrive, developmental delay, ataxia and multiorgan involvement (Rahman, 2012). Whilst none are yet treatable, some are associated with a higher risk of potentially fatal adverse liver reactions with commonly used AEDs, such as valproate. Raised serum and/or CSF lactate may be another clue, but in the acute setting, is non-specific. Diagnosis is based on genetic testing, initially using blood to identify common mutations, but not infrequently, a muscle sample is required for genetic and biochemical analysis. Everolimus for tuberous sclerosis complex (TSC). The mTOR inhibitor (mammalian Target of Rapamycin), everolimus, which has been used for various benign tumours associated with TSC for some years, has more recently been licensed for the treatment of drug-resistant epilepsy associated with TSC (French et al., 2016). As well as monitoring of serum levels to determine appropriate dose, adverse events include hyperglycaemia, hypercholesterolaemia, hypertriglyceridemia, and worsening of proteinuria requiring regular monitoring on initiation and throughout treatment, alongside standard haematological, bone health, renal and liver function tests. Other genetic testing. Epilepsy genetics is a rapidly developing field and has not been covered in this article, but is becoming increasingly relevant in specialist practice both for diagnosis and drug development, and in some instances with respect to informing treatment choices. This has been recently reviewed elsewhere (Myers et al., 2019). CONCLUSIONS Laboratory investigations, whilst not essential to the diagnosis of seizures or epilepsy, can be fundamental to determining the cause and guiding management. Over 50% of first seizures have an acute symptomatic cause, including a range of metabolic, toxic or infectious causes. The same triggers can precipitate status epilepticus, either de novo or as part of a deterioration of control in individuals with established epilepsy. Some, such as hypoglycaemia or severe hyponatraemia can be fatal without prompt identification and treatment. Failure to identify seizures associated with recreational drug or alcohol misuse can lead to inappropriate AED treatment, as well as a missed opportunity for more appropriate intervention. In individuals with established epilepsy on treatment, some laboratory monitoring is desirable at least occasionally, in particular, in relation to bone health, as well as in situations where changes in AED clearance or metabolism are likely (extremes of age, pregnancy, comorbid disorders of renal or hepatic function). For any clinician managing people with epilepsy, awareness of the commoner derangements associated with individual AEDs is essential to guide practice. A very broad range of neurometabolic disorders can be associated with epilepsy, which may manifest as a presenting feature. Awareness of suggestive clinical features and onward referral to specialist centres is recommended, though in resource-poor settings, trials of dietary treatments or supplements may be appropriate as a first step. SUPPLEMENTARY DATA Summary didactic slides are available on the www.epilepticdisorders.com website. DISCLOSURES Prof. Cock reports personal fees from Sage Pharmaceuticals Ltd, personal fees from Eisai Europe Ltd, personal fees from UCB Pharma Ltd, personal fees from European Medicines Agency, personal fees from UK Epilepsy Nurse Specialist Association, non-financial support from Special Products Ltd, grants from U.S NIH Institute of Neurological Disorders and Stroke, non-financial support from International League Against Epilepsy, E-learning Task Force, non-financial support from European Academy of Neurology, and personal fees from Bial and Eisai, Novartis, and GW Research Ltd, outside the submitted work. Dr. von Oertzen reports grants, personal fees and non-financial support from Novartis Phama, personal fees from Roche Pharma, personal fees from Biogen Idec Austria, personal fees from Liva Nova, grants from Grossegger & Drbal GmbH, grants from Merck, personal fees from Indivior Austria GmbH, personal fees and non-financial support from gtec GmbH Austria, personal fees and non-financial support from Boehringer-Ingelheim, personal fees from Philips , personal fees and non-financial support from UCB Pharma, personal fees from Almirall , personal fees from Eisai, outside the submitted work; he is webeditor in chief of the European Academy of Neurology (EAN), co-chair of the EAN scientific panel for epilepsy, and vice-president of the Österreichische Gesellschaft für Epileptologie (Austrian ILAE chapter). Dr. Craiu reports grants from BioMarine, grants from UCB, grants from A&D pharma, outside the submitted work. Drs Sutton, Barca, Komoltsev, and Dr. Guekht report no conflicts. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License

|
Scooped by
Nesrin Shaheen
onto AntiNMDA |
No comment yet.
Sign up to comment




 Your new post is loading...
Your new post is loading...