Abstract
Background
To describe the national Danish N-methyl-d-aspartate receptor encephalitis (NMDARE) cohort.
Methods
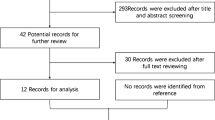
All NMDAR immunoglobulin G (IgG) positive cases in Denmark from 2009 to 2019 were included. Medical information was assessed retrospectively for clinical phenotype, workup, treatment and outcome.
Results
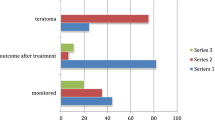
Seventy-seven patients were NMDAR IgG positive in serum/CSF. Fifty-five fulfilled the criteria of NMDARE, 18 did not and 4 had missing data. Incidence was 0.17/100,000 persons per year in 2018, and incidence rates increased since 2009. Of the 55 NMDARE patients (median age 27; 60% female), 9 had post-herpes simplex (HSE) NMDARE and 7 had a tumor (four teratomas). MRI was normal in 51% of patients. Brain FDG PET was performed in 17 patients, and was abnormal in 47% of patients with a normal MRI. First-line therapy was administered to 91%, and 24% required second-line therapy. Maintenance therapy during recovery was given 84% of patients, with no effect on relapse-risk. ICU admission occurred in 29%. Poor outcome (mRS > 2) was reported in 27% and dependent on age and etiology. Patients > 45 years had a poorer outcome (71% vs 8%, p < 0.0001), more frequently post-HSE NMDARE (47% vs 3%, p < 0.0001) and underlying malignancies (18% vs 0%).
Conclusion
The incidence of NMDARE in Denmark is currently 0.17/100,000 persons per year, and has increased since 2009. NMDARE patients in Denmark display a higher median age, lower female:male ratio, a less frequent tumor association and need for ICU admission. Maintenance therapy did not reduce relapse rate. Poor outcome was seen with higher age, likely related to underlying etiology.




Similar content being viewed by others
Data availability statement
Anonymized patient data, the statistical analysis plan and supplementary data not published within this article will be made available for purposes of replicating results by request from any qualified investigator.
References
Dalmau J et al (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7(12):1091–1098. https://doi.org/10.1016/s1474-4422(08)70224-2
Dalmau J et al (2019) An update on anti-NMDA receptor encephalitis for neurologists and psychiatrists: mechanisms and models. Lancet Neurol 18(11):1045–1057. https://doi.org/10.1016/S1474-4422(19)30244-3
Titulaer MJ et al (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12(2):157–165. https://doi.org/10.1016/s1474-4422(12)70310-1
Bien CG et al (2012) Immunopathology of autoantibody-associated encephalitides: clues for pathogenesis. Brain 135(Pt 5):1622–1638. https://doi.org/10.1093/brain/aws082
Abboud H et al (2021) Autoimmune encephalitis: proposed best practice recommendations for diagnosis and acute management. J Neurol Neurosurg Psychiatry 92(7):757–768. https://doi.org/10.1136/jnnp-2020-325300
Dalmau J, Graus F (2018) Antibody-mediated encephalitis. N Engl J Med 378(9):840–851. https://doi.org/10.1056/NEJMra1708712
McKeon G et al (2020) The patient experience of recovery following anti-NMDA receptor encephalitis: a qualitative content analysis. J Neuropsychiatry Clin Neurosci. https://doi.org/10.1176/appi.neuropsych.20030049
McKeon GL et al (2018) Cognitive outcomes following anti-N-methyl-d-aspartate receptor encephalitis: a systematic review. J Clin Exp Neuropsychol 40(3):234–252. https://doi.org/10.1080/13803395.2017.1329408
Finke C et al (2012) Cognitive deficits following anti-NMDA receptor encephalitis. J Neurol Neurosurg Psychiatry 83(2):195–198. https://doi.org/10.1136/jnnp-2011-300411
Graus F et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15(4):391–404. https://doi.org/10.1016/S1474-4422(15)00401-9
Zandi MS et al (2015) Clinical relevance of serum antibodies to extracellular N-methyl-d-aspartate receptor epitopes. J Neurol Neurosurg Psychiatry 86(7):708–713. https://doi.org/10.1136/jnnp-2014-308736
Gresa-Arribas N et al (2014) Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol 13(2):167–177. https://doi.org/10.1016/s1474-4422(13)70282-5
Hara M et al (2018) Clinical and pathogenic significance of IgG, IgA, and IgM antibodies against the NMDA receptor. Neurology 90(16):e1386–e1394. https://doi.org/10.1212/WNL.0000000000005329
Ruiz-García R et al (2021) Limitations of a commercial assay as diagnostic test of autoimmune encephalitis. Front Immunol 12:691536. https://doi.org/10.3389/fimmu.2021.691536
Vitaliani R et al (2005) Paraneoplastic encephalitis, psychiatric symptoms, and hypoventilation in ovarian teratoma. Ann Neurol 58(4):594–604. https://doi.org/10.1002/ana.20614
de Montmollin E et al (2017) Anti-N-methyl-d-aspartate receptor encephalitis in adult patients requiring intensive care. Am J Respir Crit Care Med 195(4):491–499. https://doi.org/10.1164/rccm.201603-0507OC
Zekeridou A et al (2015) Treatment and outcome of children and adolescents with N-methyl-d-aspartate receptor encephalitis. J Neurol 262(8):1859–1866. https://doi.org/10.1007/s00415-015-7781-9
Titulaer MJ et al (2014) Overlapping demyelinating syndromes and anti-N-methyl-d-aspartate receptor encephalitis. Ann Neurol 75(3):411–428. https://doi.org/10.1002/ana.24117
Martinez-Hernandez E et al (2020) Clinical significance of anti-NMDAR concurrent with glial or neuronal surface antibodies. Neurology 94(22):e2302–e2310. https://doi.org/10.1212/wnl.0000000000009239
Armangue T et al (2014) Herpes simplex virus encephalitis is a trigger of brain autoimmunity. Ann Neurol 75(2):317–323. https://doi.org/10.1002/ana.24083
Pruss H et al (2012) N-Methyl-d-aspartate receptor antibodies in herpes simplex encephalitis. Ann Neurol 72(6):902–911. https://doi.org/10.1002/ana.23689
Armangue T et al (2018) Frequency, symptoms, risk factors, and outcomes of autoimmune encephalitis after herpes simplex encephalitis: a prospective observational study and retrospective analysis. Lancet Neurol 17(9):760–772. https://doi.org/10.1016/S1474-4422(18)30244-8
Nosadini M et al (2017) Herpes simplex virus-induced anti-N-methyl-d-aspartate receptor encephalitis: a systematic literature review with analysis of 43 cases. Dev Med Child Neurol 59(8):796–805. https://doi.org/10.1111/dmcn.13448
Titulaer MJ et al (2013) Late-onset anti-NMDA receptor encephalitis. Neurology 81(12):1058–1063. https://doi.org/10.1212/WNL.0b013e3182a4a49c
Abboud H et al (2021) Autoimmune encephalitis: proposed recommendations for symptomatic and long-term management. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2020-325302
Ho ACC et al (2017) High sensitivity and specificity in proposed clinical diagnostic criteria for anti-N-methyl-d-aspartate receptor encephalitis. Dev Med Child Neurol 59(12):1256–1260. https://doi.org/10.1111/dmcn.13579
Irani SR et al (2010) N-Methyl-d-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 133(Pt 6):1655–1667. https://doi.org/10.1093/brain/awq113
Viaccoz A et al (2014) Clinical specificities of adult male patients with NMDA receptor antibodies encephalitis. Neurology 82(7):556–563. https://doi.org/10.1212/WNL.0000000000000126
Florance NR et al (2009) Anti-N-methyl-d-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol 66(1):11–18. https://doi.org/10.1002/ana.21756
Jørgensen LK et al (2017) Incidence and mortality of herpes simplex encephalitis in Denmark: a nationwide registry-based cohort study. J Infect 74(1):42–49. https://doi.org/10.1016/j.jinf.2016.09.004
Erickson TA et al (2020) Infectious and autoimmune causes of encephalitis in children. Pediatrics. https://doi.org/10.1542/peds.2019-2543
Gable MS et al (2012) The frequency of autoimmune N-methyl-d-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California Encephalitis Project. Clin Infect Dis 54(7):899–904. https://doi.org/10.1093/cid/cir1038
Dubey D et al (2018) Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann Neurol 83(1):166–177. https://doi.org/10.1002/ana.25131
Guasp M et al (2020) Clinical features of seronegative, but CSF antibody-positive, anti-NMDA receptor encephalitis. Neurol Neuroimmunol Neuroinflamm. https://doi.org/10.1212/NXI.0000000000000659
Probasco JC et al (2017) Abnormal brain metabolism on FDG-PET/CT is a common early finding in autoimmune encephalitis. Neurol Neuroimmunol Neuroinflamm 4(4):e352. https://doi.org/10.1212/nxi.0000000000000352
Solnes LB et al (2017) Diagnostic value of (18)F-FDG PET/CT versus MRI in the setting of antibody-specific autoimmune encephalitis. J Nucl Med 58(8):1307–1313. https://doi.org/10.2967/jnumed.116.184333
Yuan J et al (2016) Changing brain metabolism patterns in patients with ANMDARE: serial 18F-FDG PET/CT findings. Clin Nucl Med 41(5):366–370. https://doi.org/10.1097/RLU.0000000000001164
Ganesh A, Bartolini L, Wesley SF (2020) Worldwide survey of neurologists on approach to autoimmune encephalitis. Neurol Clin Pract 10(2):140–148. https://doi.org/10.1212/CPJ.0000000000000701
McKeon GL et al (2016) Cognitive and social functioning deficits after anti-N-methyl-d-aspartate receptor encephalitis: an exploratory case series. J Int Neuropsychol Soc 22(8):828–838. https://doi.org/10.1017/s1355617716000679
Acknowledgements
This research was conducted using the Danish National Biobank resource, supported by the Novo Nordisk Foundation. Authors acknowledge the Autoimmune Laboratory at the Dept. of Clinical Immunology, Odense University Hospital and the Autoimmune Laboratory at Statens Serum Institut, Denmark. In addition, all the involved hospitals who kindly provided clinical information on patients.
Funding
MSN received grant support by Odense University Hospital and the Faculty of Health Sciences, University of Southern Denmark. No award/grant number.
Author information
Authors and Affiliations
Contributions
Design and conceptualization: MB and MSN. Acquisition of data: MSN, MSØ, MR, ACN, and ML. Analysis and interpretation of the data: MSN and MB. Drafting and revising the manuscript: MSN, MSØ, ACN, MR, ML, and MB.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Standard protocol approvals, registrations, and patient consents
Approval was obtained from the Danish Data Protection Agency and the Danish Medical Authorities (3–3013-3124/1), who granted a waiver for patient consent.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nissen, M.S., Ørvik, M.S., Nilsson, A.C. et al. NMDA-receptor encephalitis in Denmark from 2009 to 2019: a national cohort study. J Neurol 269, 1618–1630 (2022). https://doi.org/10.1007/s00415-021-10738-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10738-9