 Your new post is loading...

|
Scooped by
rob halkes
|
Free White Paper to Top 5 Medical Device Industry Trends in 2018 Digital device technology continues to move at a fast pace, which means device manufacturers should keep a close watch on emerging trends and be ready to adapt to new ideas and methodologies.
• Trend #1: Software in Medical Devices Will Become More Common — and Complex
"The benefits of innovative technology to both providers and patients are exponential. However, given the complexity of technology in devices, manufacturers will need to revamp some of their approaches to design and development. This includes devoting even more time and effort at the onset of device planning — particularly design control, risk management and cybersecurity." ...
• Trend #2: Atypical Medical Device Technology Will Become More Typical - Communication needs to be inclusive and on record - Having a device doesn’t always mean it gets used right away.. "health care providers need to adopt their clinical processes to work with medical devices. Developers of medical devices and products should consider pacing themselves with new device technologies as some devices may require providers to customize their workflows around using them. Some providers may be hesitant to do this until there is a wider need for a device. • Trend #3: Medical Device Industry Will Experience More Challenges with “Proving” Compliance
Device manufacturers will face challenges in demonstrating compliance as the medical device industry continues to experience ongoing changes and updates to regulations, guidelines and reciprocating conditions... According to the FDA, a mobile app that serves as an accessory to support, supplement or augment an existing medical device, or to transform a mobile platform for some form of medical use is now considered an FDA- regulated mobile medical app. The FDA will use the same risk-based approach to ensure the safety and effectiveness of mobile apps that it uses for other medical devices. ...
The International Medical Device Regulators Forum (IMDRF) is currently implementing a medical device single audit program (MDSAP). • Trend #4: Regulatory Authorities Will Continue to Emphasize Human Factors Engineering Human factors engineering (HFE) is a regulatory requirement intended to reduce medical device use errors and develop more user-friendly and intuitive devices. Human factors is part of robust design controls for medical devices. The push toward reducing or eliminating user errors includes ANSI/AAMI/IEC 62366, which focuses on the safety aspects of usability engineering.... Certain human factors issues can only be validated in the actual use environment because simulated use testing might not be sufficient.... • Trend #5: De Novo Pathway Will Become Easier and Faster The number of successful de novo classifications is on the rise. This is due in part to the FDA streamlining the application process by no longer requiring a 510(k) and a not substantially equivalent (NSE) determination. The “De Novo Classification Process (Evaluation of Automatic Class III Designation” guidance states “If a person believes their device is appropriate for classification into Class I or Class II and determines, based on currently available information, there is no legally marketed predicate device, they may submit a De Novo request without a preceding 510(k) and NSE.” The de novo pathway is risk-based, so a strong risk mitigation strategy is key.

|
Scooped by
rob halkes
|
Bringing together patients' perspectives on eHealth and mHealth -
WE NOW INVITE YOU ... It is exactly one year since the launch of myhealthappsblog.com, which brings together patient views on eHealth (health/healthcare using electronic channels) and mHealth (health/healthcare using mobile phones). The blog also supports the website myhealthapps.net, which curates over 500 health apps recommended by patients and patient groups. The aim of the myhealthapps blog is to: - Highlight best practice in health app development, mHealth and eHealth from the patient perspective.
- Focus the attention of app developers on the unmet health needs of the public, patients, and carers.
- Bridge the gap between the public, patients, and carers, and app developers—with the intention of improving the relevance and quality of health apps, mHealth and eHealth as well as their impact upon the health of users and in healthcare systems.
To submit your own blog, which can be on any subject related to eHealth and mHealth in your area of interest-as long as it involves a patient or patient group perspective. Instructions and terms and conditions for submission are found at the end of this email. You can submit you blog by filling out the following online form: https://www.surveymonkey.co.uk/r/yourblog Myhealthappsblog.com is moderated.
Please read the Blog Guidelines and Terms & Conditions [at the end of this email] for more details. Happy blogging! _________ Thank you.
If you have any technical issues, please contact dee@patient-view.com
If you are interested in finding out more about PatientView reports and research, please contact Alex Wyke at alexwyke@patient-view.com, or Dee O’Sullivan for myhealthapps’ activities at dee@patient-view.com
Blogging Guidelines
1. Blogs and social media are all about engagement, so think about what impact you want to make – start a conversation!
2. Have a clear goal. For example, do you want to comment on what impact a particular issue or policy has on a patient/carer community? Or do you want to promote particular campaigns or activities, related to patient perspectives in this field? Or do you want to share a powerful patient stories on personal health experiences?
3. Have a compelling title.
4. Be aware of people’s right to privacy. If you name people in your post, check you have their permission to mention them.
5. Graphics or photos will make your post more powerful and engaging.
6. Don’t forget to include a call for action or next steps, if relevant – eg, links to attend an event, take part in research, share the post, sign a petition etc.
Terms & Conditions
1. Please check out our guidelines for guest bloggers.
2. If you are not writing in your own name but on behalf of a patient group, we will still need to have your contact details so we can follow up with you on the post if needed. These will not be uploaded with the post unless you agree.
3. We may edit posts for length if necessary and also for language if deemed disrespectful or unlawful.
4. We will endeavour never to misrepresent the messages of our guest bloggers whose posts we publish.
5. We will also check posts for relevance to our subject areas and reserve the right not to publish.
6. Once you’ve submitted your post, we will send you a confirmation email that your submission has been received. It may take time for your post to be published. We appreciate your patience.
7. If you have any questions please email dee@patient-view.com. ALL submissions need to be submitted via the form above.
Social Media Compliance in Health Care By Eric Newman, JD, CCEP, CHPC ¶53,150 Introduction business associates. “Covered entities” are health care providers (e…
Via Plus91
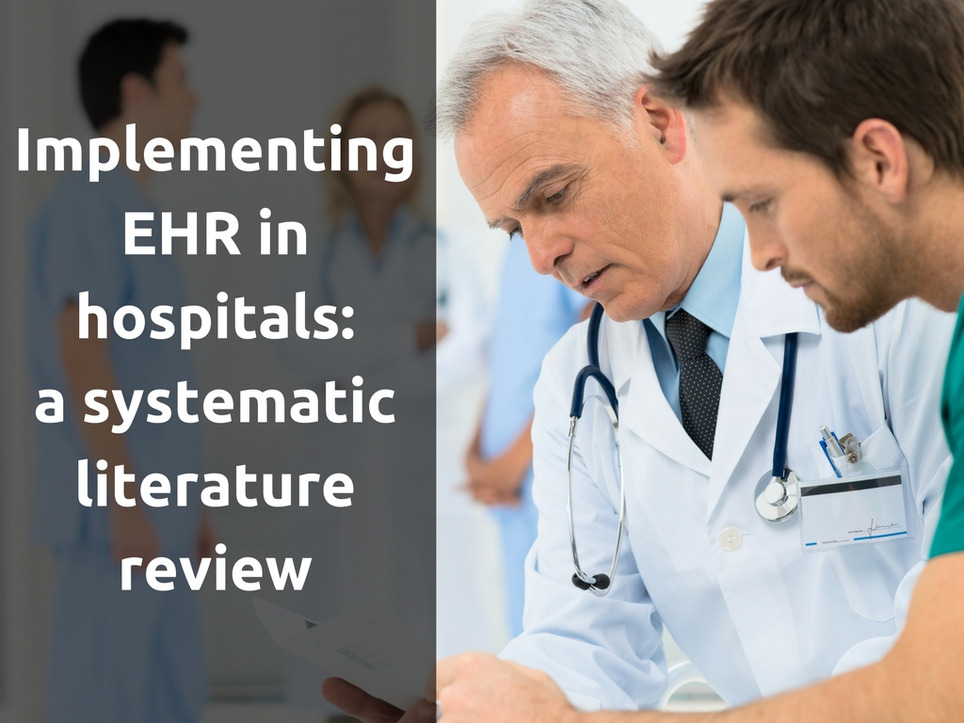
Background The literature on implementing Electronic Health Records (EHR) in hospitals is very diverse. The objective of this study is to create an overview of the existing literature on EHR implementation in hospitals and to identify generally applicable findings and lessons for implementer. Methods A systematic literature review of empirical research on EHR implementation was conducted. Databases used included Web of Knowledge, EBSCO, and Cochrane Library. Relevant references in the selected articles were also analysed. Search terms included Electronic Health Record (and synonyms), implementation, and hospital (and synonyms). Articles had to meet the following requirements: written in English, full text available online, based on primary empirical data, focused on hospital-wide EHR implementation, and satisfying established quality criteria. Results Of the 364 initially identified articles, this study analyses the 21 articles that met the requirements. From these articles, 19 interventions were identified that are generally applicable and these were placed in a framework consisting of the following three interacting dimensions: EHR context, EHR content, and EHR implementation process. Conclusions Although EHR systems are anticipated as having positive effects on the performance of hospitals, their implementation is a complex undertaking. This systematic review reveals reasons for this complexity and presents a framework of 19 interventions that can help overcome typical problems in EHR implementation. This framework can function as a reference for implementer in developing effective EHR implementation strategies for hospitals.
Via Lionel Reichardt / le Pharmageek

|
Scooped by
rob halkes
|
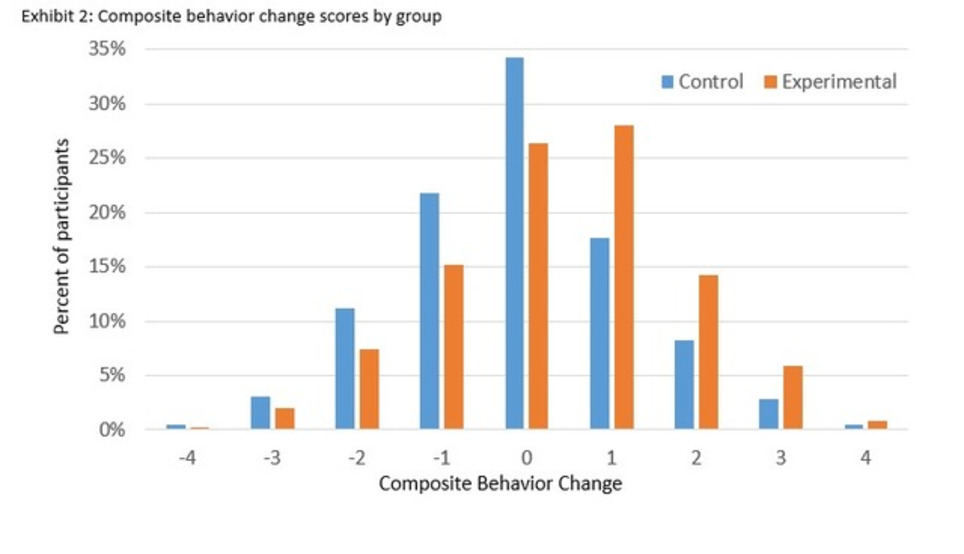
Journal of Medical Internet Research - International Scientific Journal for Medical Research, Information and Communication on the Internet ABSTRACT Background: In low/middle income countries like India, diabetes is prevalent and health care access limited. Most adults have a mobile phone, creating potential for mHealth interventions to improve public health. To examine the feasibility and initial evidence of effectiveness of mDiabetes, a text messaging program to improve diabetes risk behaviors, a global nonprofit organization (Arogya World) implemented mDiabetes among one million Indian adults. Objective: A prospective, parallel cohort design was applied to examine whether mDiabetes improved fruit, vegetable, and fat intakes and exercise. Methods: Intervention participants were randomly selected from the one million Nokia subscribers who elected to opt in to mDiabetes. Control group participants were randomly selected from non-Nokia mobile phone subscribers. mDiabetes participants received 56 text messages in their choice of 12 languages over 6 months; control participants received no contact. Messages were designed to motivate improvement in diabetes risk behaviors and increase awareness about the causes and complications of diabetes. Participant health behaviors (exercise and fruit, vegetable, and fat intake) were assessed between 2012 and 2013 via telephone surveys by blinded assessors at baseline and 6 months later. Data were cleaned and analyzed in 2014 and 2015. Results: 982 participants in the intervention group and 943 in the control group consented to take the phone survey at baselne. At the end of the 6-month period, 611 (62.22%) in the intervention and 632 (67.02%) in the control group completed the follow-up telephone survey. Participants receiving texts demonstrated greater improvement in a health behavior composite score over 6 months, compared with those who received no messages F(1, 1238) = 30.181, P<.001, 95% CI, 0.251-0.531. Fewer intervention participants demonstrated health behavior decline compared with controls. Improved fruit, vegetable, and fat consumption (P<.01) but not exercise were observed in those receiving messages, as compared with controls. Conclusions: A text messaging intervention was feasible and showed initial evidence of effectiveness in improving diabetes-related health behaviors, demonstrating the potential to facilitate population-level behavior change in a low/middle income country. Trial Registration: Australian New Zealand Clinical Trials Registry (ACTRN): 12615000423516; https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=367946&isReview=true (Archived by WebCite at http://www.webcitation.org/6j5ptaJgF) J Med Internet Res 2016;18(8):e207

|
Scooped by
rob halkes
|
Even though the concept of telemedicine has been floating around for decades, it is only really beginning to soar as of late. Why, if we had this revolutionary concept right underneath our noses, are we just beginning to utilize it? There are many reasons for this, some of which include: - Technological growth is perhaps the primary reason telemedicine is finally getting its due. With all our modern advancements, the digital stage is now set for telemedicine to shine. With faster internet connections, wi-fi available almost anywhere and better software being manufactured, a video conference is as smooth as butter nowadays. Can you imagine having a video chat back when dial-up was commonplace?
- Privacy concerns are finally being eradicated. Great strides have been made in the arena of privacy and patient information protection so that people can confidently access online care without the worries that existed years ago. ...
- Reluctance on part of doctors and patients to welcome change and advance with the times has prevented telemedicine from flourishing for decades. Luckily that is finally starting to change.
- Obstacles like legality, software development and logistics are only now being ironed out and surmounted. Telemedicine was used broadly before, but now has the potential to be used in very detailed ways that suit patients much better.
- Insurance companies like Medicaid are finally opening the door to let telemedicine in. They are beginning to recognize and accept the growing popular demand of telemedicine healthcare.
- Smartphones and tablets are opening up possibilities by making healthcare accessible virtually anywhere. Gone are the days of bulky stationary desktops. Now there are telemedicine apps available to allow people to see doctors from anywhere.
- Baby boomers are less mobile now and more ‘tech-savvy’ than ever, so even though people think of millennials as the primary users for telemedicine, don’t discount the baby boomers! Older Americans aged 60+ comprise the fastest growing social media demographic, and are getting hip to all kinds of digital trends and opportunities.
- The state of the healthcare system has patients frustrated and finally seeking alternatives to crowded germy waiting rooms. People are noticing that certain problems can be circumvented by telemedicine such as travel, wait-times and exposure to germs.
- Healthcare costs can be effectively slashed by utilizing telemedicine as well. ...! You can avoid travel costs as well as lost work days by using telemedicine.
- Triage effectivity. Telemedicine offers an excellent mode of triaging non-critical medical issues. This can cut down on ER congestion countrywide as well as mistakes made by overworked doctors. People are starting to see that they needn’t cart their sick selves all the way to the ER or a clinic to wait around for a prescription that can be obtained in their very own living rooms.
Well that’s our look at why telemedicine was waiting in the wings until now! Thanks1

|
Scooped by
rob halkes
|
Editorial from BMJ
Social Media and Healthcare quality improvement: a nascent filed Two articles1 ,2 describe the use of social media to describe or potentiate healthcare quality improvement. Taken together, these articles point to an exciting—but still nascent—trend. We hope that these two pilot studies will be taken as a call to future research rather than as definitive reports. The first article1 describes the proportion of emergency department (ED) patients who consent for researchers to download their Facebook and Twitter data. The novelty of this study lies in its underlying premise: accessing patients’ social media data could, in theory, permit better awareness of patients’ health status and risks, and thereby permit real-time interventions and improved patient engagement. To our knowledge, this study is the first to show the acceptability, feasibility and limitations of accessing patients’ social media data. It thereby gives hope that incorporating social feeds into healthcare may be possible.[...]
The second article, ‘Measuring patient-perceived quality of care in U.S. hospitals using Twitter’2 extends others’ work using social media to measure or evaluate healthcare. Twitter has previously been shown to provide real-time monitoring of conditions such as viral and foodborne illness,5 mental illness6 and substance use.7 ,8 The study by Hawkins et al,2 showing a correlation between patient sentiment and readmission rates, has findings that are similar to Kilaru et al's9 recent article in this journal that analysed Yelp reviews. While these methods provide insight into a variety of patient characteristics and behaviours, they are nonetheless limited and subject to misinterpretation. [...]
Another major limitation for both of these articles is that we still have problems accurately interpreting the meaning of social media. [...] Finally, both articles touch on—but do not provide answers to—the spectre of privacy. In the first paper, among the 50% willing to engage in discussion, privacy was the primary reason for people refusing to share their data. The authors note that in general, public supports purpose of using social media data for health research, accepting it without consent (compared with their lack of support for marketing research, done with their consent)—but this paper suggests attitudes change when it's an individual's data that's being requested, during that individual's emergency. These findings are similar to those of others’ findings regarding patients’ privacy preferences for electronic health information.13 [...] All of these limitations aside, we are enthused by these papers. Together, they help lay the foundation for further efforts integrating social media into electronic health record (EHR) and healthcare... See it in pdf

|
Scooped by
rob halkes
|
For a growing number of people, the main way to communicate with people, both personally and professionally, is through their smartphones. While digital communication has become widely accepted, there is one place where its adoption is lagging: health care. U.S. News and World Report points to a Nielsen survey that shows that the vast majority of medical professionals in the United States do not use e-mail or text messages to communicate with their patients. Physicians welcome new forms of technology in their practices, and smartphones seem like a logical way to improve patient engagement, patient adherence, and patient empowerment. So why don’t more doctors text or e-mail their patients? The fact of the matter is that the reluctance of physicians to embrace digital communications with their patients has little to do with technology. Doctors want to offer the best possible care for their patients but, like anyone who provides a service, they also want to be paid for it. Doctors can easily submit a claim for an office visit or a medical procedure but, as U.S. News explains, the insurance system is not currently set up to reimburse a doctor’s digital communication with his or her patients. But that is starting to change, healthcare reform has shifted insurance models toward compensating doctors for the quality of the care, as well as patient outcomes. But insurers still need to formally recognize these communication changes. Regulatory restrictions are another barrier to doctor/patient digital communication. Under the federal Health Insurance Portability and Accountability Act, healthcare providers must take steps to ensure the privacy of patient information. Some forms of digital communication are just not secure enough to meet HIPAA requirements. With some effort, a physician can find a telecommunications and software services that meet federal security requirements, but the burden is on the physician to find these providers. Even though digital communication with patients has a long way to go, changes are on the way. Demand is driving the IT sector to develop new technological solutions. “The generation of young and digitally native doctors will help expedite this process,” U.S. News says. While digital communication has become widely accepted, there is one place where its adoption is lagging: health care.

|
Scooped by
rob halkes
|
Dignity Health, announced results from a randomized controlled study which demonstrated that the use of digital health technology improved asthma control. The study, “Effectiveness of Population Health Management Using the Propeller Health Asthma Platform: A Randomized Clinical Trial,” was recently published in the Journal of Allergy and Clinical Immunology: In Practice. The Propeller Health Asthma Platform utilizes sensors, mobile applications, and analytics to monitor short-acting β-agonist (SABA) and inhaled corticosteroid use in real-time. The platform provides detailed information about patterns of medication use and notifications about patients with worsening asthma control. “The research demonstrates that the benefits of telehealth go beyond monitoring medication adherence, but can also identify patterns of risk and impairment. This additional information may allow more timely interventions and enhanced asthma management,” said Dr. Rajan Merchant, the principal study investigator and physician at Dignity Health’s Woodland Clinic Medical Group. “Although additional study efforts are needed, digital health is promising to help improve care and asthma control.” Currently, more than 40 percent of both adults and children in the U.S. report uncontrolled asthma, according to recent studies. Current guidelines recommend monitoring of SABA use and assessment of asthma control. Electronic monitoring of SABA use provides an indication of poor asthma control. More than 495 adults and children enrolled in this study. The results found that the total amount of SABA use, and the total number of days when SABA was needed, was lower in the group using the Propeller Health Asthma Platform compared to the patients receiving routine care. Furthermore, a significantly greater increase in the Asthma Control Test was demonstrated in adults with uncontrolled asthma in the intervention group compared to adults with uncontrolled asthma under routine care.

|
Scooped by
rob halkes
|
HIMSS study shows telemedicine software solutions poised for growth in 2016
Originally posted on Nov, 2015
Although organizations in the United States are still trying to optimize the use of current telehealth solutions, telehealth is undoubtedly poised for continued growth in the U.S. (and many other countries as well). Telemedicine is gaining momentum as it has proven to increase access to care and reduce costs via teleconsultations and remote patient monitoring. U.S. consumers are beginning to use wearable devices to track and collect their personal health data. Over time, we will see more of a willingness to share that data with healthcare providers and intermediaries. The Healthcare Information and Management Systems Society (“HIMSS”) conducted a survey on telemedicine adoption in the United States. The survey polled 276 healthcare decision makers and physician executives. Brendan FitzGerald, research director at HIMSS Analytics, discussed the results with some of us last week. Here are some highlights of the survey’s findings, of those engaged in telemedicine: - 70% utilize a two-way videoconferencing system.
- 57% use a hub and spoke model (audio/visual only between originating sites)
- 49.7% are using a patient portal or application-focused patient engagement (services delivered via portal with mobile or desktop access)
- 20% utilize concierge services (i.e. eVisits and online consults)
- The number of respondents engaged in remote patient monitoring in the home decreased from 38% in 2014 to 30% in 2015.
- 52% are still uncertain about future investment in telemedicine; 28% polled are not increasing their current investment; 20% are planning on future investment on top of their current program.
- 26% are planning to expand their telemedicine programs to add other specialties in the near future.
- 34% are engaged in telemedicine primarily to develop a service that increases access and integrates care across rural areas; 22% are focused on developing a service that reduces overall costs for their organization; 18% are seeking to develop specialty services not otherwise available in the region.
The HIMSS Analytics survey can be found here. You can contact ABISA, a consultancy specializing in solo and small group practice management by visiting them at ABISALLC.com. Link to original post

|
Scooped by
rob halkes
|
Conclusions: A telemedicine-based symptom reporting program facilitated early treatment of symptoms and improved lung function and functional status.
Background: Patients with chronic obstructive pulmonary disease (COPD) may not recognize worsening symptoms that require intensification of therapy. They may also be reluctant to contact a healthcare provider for minor worsening of symptoms. A telemedicine application for daily symptom reporting may reduce these barriers and improve patient outcomes.
Materials and Methods: Patients hospitalized for a COPD exacerbation within the past year or using supplemental O2 were approached for participation. Patients received optimal COPD care and were given a telecommunication device for symptom reporting. Initial symptom scores were obtained while patients were in their usual state of health. Patients were randomly assigned to an intervention group or a control group (usual medical care). The control group patients were instructed to seek medical care if their condition worsened. The intervention group symptom scores were assessed by a computer algorithm and compared with initial values. Scores 1 or more points above the initial score generated an “alert,” and patients were reviewed by a nurse and referred to a physician who prescribed treatment. Results: Eighty-six patients were screened; 79 met entry criteria and were randomized (intervention group, n=39; control group, n=40). Twelve patients submitted five or fewer symptom reports (5 intervention; 7 control) and were excluded from the analysis. Daily peak flow and dyspnea scores improved only in the intervention group. There were no differences in hospitalization and mortality rates between groups. No serious adverse events were reported.

|
Scooped by
rob halkes
|
Conclusions: Caregivers of children with special healthcare needs have notable levels of psychosocial challenges and those challenges are associated with their e-health resource seeking. Although e-health interventions, including ones that focus on child health education and caregiver support, may be the future of healthcare, a concerted effort is needed to educate caregivers about the benefits of e-health.
Objectives: In this study, we explored the relationships between the psychosocial health of caregivers of children with special healthcare needs and their e-health use. Additionally, the analysis examined moderating effects of a caregiver's perceptions of e-health and his or her e-health literacy on the associations among four domains of psychosocial health and e-health use. Materials and Methods: To date, 313 caregivers of children, 12–18 years of age, with special healthcare needs have been recruited. Covariate-adjusted multivariable regressions determined associations between psychosocial health domains of caregivers and e-health use. E-health literacy and perceptions of e-health were further tested as moderators of the relationship between psychosocial health and e-health use. Results: Among the caregiver population, 31% had problems with social functioning, 36.1% with communication, 43.3% with family relationships, and 46.3% with worrying for their child. After adjusting for demographic variables, e-health use was associated with poorer levels of social functioning, communication, worry, and family relationship.
E-health use was also associated with e-health literacy. Perceptions of e-health significantly moderated the relationships among social functioning, communication, and e-health, with the relationship being significantly stronger in caregivers with more positive perceptions of e-health.

|
Scooped by
rob halkes
|
The same forces that have made instant messaging and video calls part of daily life for many Americans are now shaking up basic medical care.
TACOMA, Wash. — One night, when her face turned puffy and painful from what she thought was a sinus infection, Jessica DeVisser briefly considered going to an urgent care clinic, but then decided to try something “kind of sci-fi.”
She sat with her laptop on her living room couch, went online and requested a virtual consultation. She typed in her symptoms and credit card number, and within half an hour, a doctor appeared on her screen via Skype. He looked her over, asked some questions and agreed she had sinusitis. In minutes, Ms. DeVisser, a stay-at-home mother, had an antibiotics prescription called in to her pharmacy. Continue reading the main story
The same forces that have made instant messaging and video calls part of daily life for many Americans are now shaking up basic medical care. Health systems and insurers are rushing to offer video consultations for routine ailments, convinced they will save money and relieve pressure on overextended primary care systems in cities and rural areas alike. And more people like Ms. DeVisser, fluent in Skype and FaceTime and eager for cheaper, more convenient medical care, are trying them out [..] But telemedicine is facing pushback from some more traditional corners of the medical world. Medicare, which often sets the precedent for other insurers, strictly limits reimbursement for telemedicine services out of concern that expanding coverage would increase, not reduce, costs. Some doctors assert that hands-on exams are more effective and warn that the potential for misdiagnoses via video is great [..]. While telemedicine consultations have been around for decades, they have mostly connected specialists with patients in remote areas, who almost always had to visit a clinic or hospital for the videoconference. The difference now is that patients can be wherever they want and use their own smartphones or tablets for the visits, which are trending toward more basic care.[..] Advocates say virtual visits for basic care could reduce costs over the long term. It is cheaper to operate telemedicine services than brick-and-mortar offices, allowing companies to charge as little as $40 or $50 for consultations — less than for visits to emergency rooms, urgent care centers and doctors’ offices. They also say that by letting people talk to a doctor whenever they need to, from home or work, virtual visits make for more satisfied and potentially healthier patients than traditional appointments that are available only at certain times.[..] ...When the doctor appeared on her screen, she told him her symptoms and, holding her iPad close to her face, showed him her painful tooth and the swelling in her jaw. “I was in so much pain, I didn’t care that it was weird,” Ms. Sickmeier said. “He got right to the point, which was what I wanted. He prescribed antibiotics and called them into an all-night pharmacy about 20 minutes away.” Washington State gave a victory to the industry in April when Gov. Jay Inslee, a Democrat, signed legislation requiring insurers to cover a range of telemedicine services if they already cover those services when provided in person. But the new law, which made Washington the 24th state to ensure reimbursement for some telemedicine services, does not cover virtual urgent care outside a medical facility.
Still, the law “opens the doors with a lot of our payers,” said Matt Levi, CHI Franciscan Health’s director of virtual health services. He added that some insurers, like Molina Healthcare of Washington, the state’s largest Medicaid plan, were starting to cover virtual urgent care, though the law does not require it. [...]
Some large insurers are starting to pay, too. UnitedHealthcare, the nation’s largest insurer, announced in April that it would cover virtual visits for most of its 26 million commercial members by next year, citing the shortage of primary care doctors and the cost of less than $50 per virtual visit.[...] Virtual urgent care visits are undoubtedly less expensive than trips to the emergency room, said Dr. Ateev Mehrotra, a professor of health policy at Harvard Medical School, who has studied telemedicine.[..] CHI Franciscan’s virtual urgent care program contracts with Carena, a private company in Seattle that employs 17 physicians and nurse practitioners to do virtual consultations in 11 states. Among CHI Franciscan’s patients, the most frequent users are women ages 25 to 55, and the most typical diagnoses are bladder infections, upper respiratory tract infections and pinkeye. Users are prescribed medication about 40 percent of the time, said Beth Bacon, the company’s vice president for consumer affairs. Most visits take place on weekends or between 5 p.m. and 8 a.m., she said, when doctors’ offices are closed. Like other virtual urgent care programs, CHI Franciscan’s emphasizes that it is not for medical emergencies, advising customers on its website to “call 911 or proceed to the nearest emergency room” if they have chest pain, difficulty breathing or other potentially life-threatening symptoms. Continue reading the main story

|
Scooped by
rob halkes
|
Forty-one percent of consumers have never heard of telemedicine, according to a new survey of 1,200 consumers conducted by Survey Sampling International on behalf of HealthMine. That number goes down for millennials, just 30 percent of whom say they haven’t heard of telemedicine, but it goes up for the 45 to 64 age group, 46 percent of whom hadn’t heard of telemedicine. HealthMine is a consumer health engagement company, and as such has a stake in gauging consumer awareness of health technology trends. “Telemedicine has the potential to deliver convenient and affordable basic healthcare to people of all ages,” Bryce Williams, CEO and President of HealthMine said in a statement. “Wellness programs can be the place where consumers are educated on the best way to access healthcare services, whether it be through a doctor’s office, emergency room, urgent care center, or telemedicine visit. Plus, telehealth is evolving to more than telephone visits. Soon, your smartphone will be a stethoscope and more.” In the survey consumers were asked whether they would use telemedicine if it was offered by their physician as an alternative to traditional doctor visits, and whether they understood when it was best to use telemedicine. For the second question, “I’ve never heard of telemedicine” was included as a response option. Overall, 45 percent of respondents said they would use telemedicine if it was offered, 16 percent said they wouldn’t, and 39 percent weren’t sure. The number who said they would use telemedicine rose to 58 percent for millennials (25 to 34-year-olds) and dropped to 37 percent for 55 to 64-year-olds. However the difference was mostly in how many were unsure — the portion of each group that answered “no” was 15 percent for millennials, 17 percent for seniors, and 16 percent for all age groups in between. Forty-three percent of total respondents said they knew when it was best to use telemedicine, 16 percent said they didn’t, and 41 percent said they hadn’t heard of telemedicine. Fifty-two percent of millennials and 46 percent of 35 to 44-year-olds felt they knew when to use telemedicine compared to 38 percent of 55 to 64-year-olds and just 34 percent of 45 to 54-year-olds. Earlier this month, a 500-person survey from TechnologyAdvice found that some 35 percent of consumers said they would likely choose a virtual visit over an in-person one. The survey also found that 56 percent of respondents would be somewhat or very uncomfortable conducting a doctor visit using a telemedicine offering. On the other hand, 75 percent of people said they would not trust a diagnosis that a doctor made over a video visit, or would trust it less than if they met with a doctor in person.

|
Scooped by
rob halkes
|
Rely on Curely for everyday health concerns Watch Video HOW IT WORKS Curely brings board-certified doctors around the world to your fingertips. CHOOSE YOUR DOCTOR Browse through a list of board-certified doctors and select your doctor by specialty, price, and language. DISCUSS YOUR CONCERNS WITH YOUR DOCTOR Chat with a doctor immediately or send a …

|
Scooped by
rob halkes
|
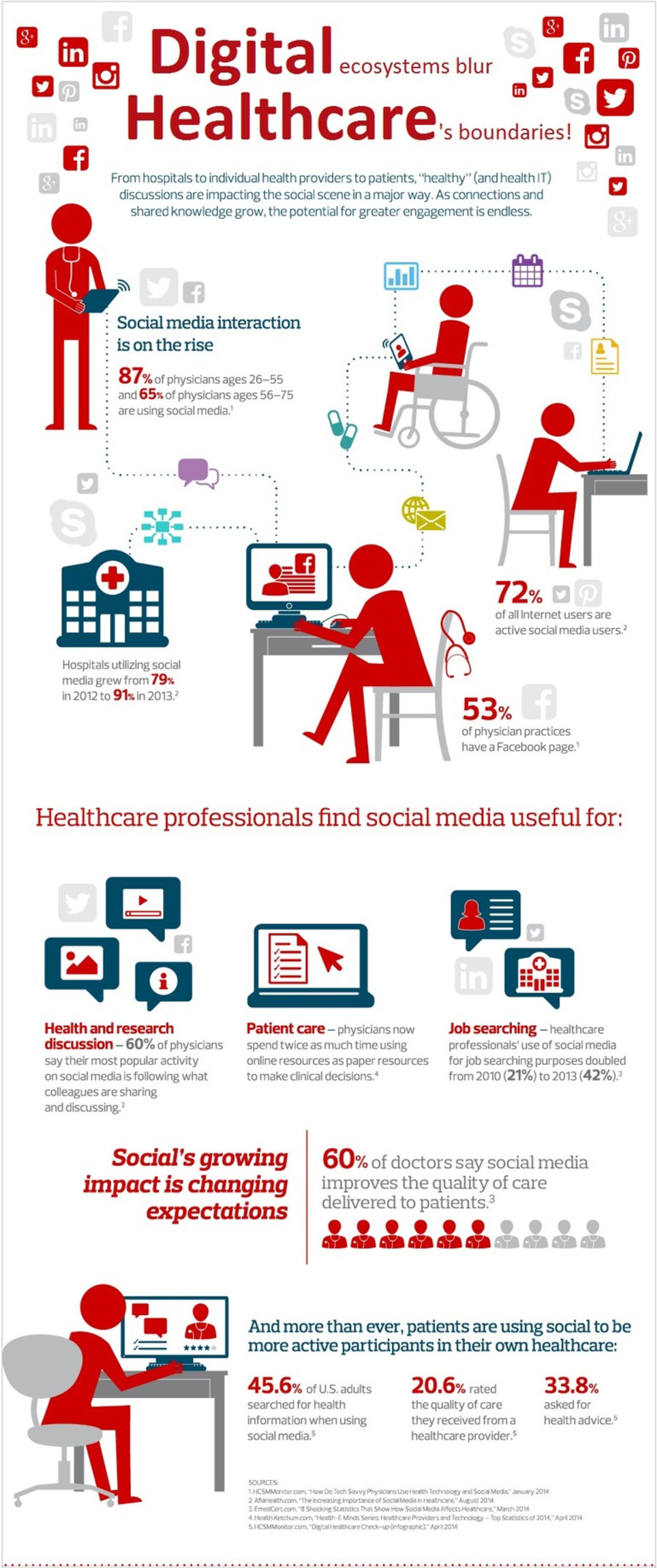
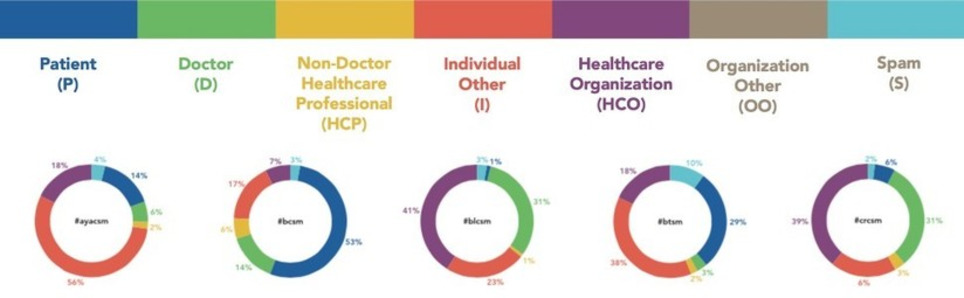
Health Hashtags Research - Can We Make It Work? People deserve access to safe, reliable health information online. Doctors have an ethical obligation to help make the internet easier and safer. Will health hashtags help or not? On June 1st, I presented data on the growing use of the Cancer Tag Ontology (CTO) at the American Society of Clinical Oncology’s annual meeting. Here is the poster:
Analyzing 531,765 tweets from over 70,000 users through December 2014, we found that CTO use is increasing. 93% still come from tags with active chats. We didn’t do any formal statistical analysis, but it’s interesting to see how each tag has different stakeholders using them. At the meeting, ASCO attendees from all backgrounds expressed interest and came to the poster: patients, advocacy organizations, doctors, industry. Beyond the scope of the study, I learned more from discussion with Symplur: as of early May, 62% of NCCN-designated cancer centers have used CTO tags at least 25 times. The five biggest users: Dana-Farber Cancer Institute, MD Anderson Cancer Center, Lurie Comprehensive Cancer Center, Memorial Sloan-Kettering Cancer Center, and UCSF Medical Center. Despite the great response, we need more research on whether hashtags help. Originally, I focused on creating meaning and community-building by patients and advocates. Collaboration with doctors like Deanna Attai has worked great for #bcsm, but #pancsm was started by doctors. It has been active and useful, just different. What will work best? Read on here: Symplur

|
Scooped by
rob halkes
|
Abstract The telemedicine intervention in chronic disease management promises to involve patients in their own care, provides continuous monitoring by their healthcare providers, identifies early symptoms, and responds promptly to exacerbations in their illnesses. This review set out to establish the evidence from the available literature on the impact of telemedicine for the management of three chronic diseases: congestive heart failure, stroke, and chronic obstructive pulmonary disease. By design, the review focuses on a limited set of representative chronic diseases because of their current and increasing importance relative to their prevalence, associated morbidity, mortality, and cost. Furthermore, these three diseases are amenable to timely interventions and secondary prevention through telemonitoring. The preponderance of evidence from studies using rigorous research methods points to beneficial results from telemonitoring in its various manifestations, albeit with a few exceptions. Generally, the benefits include reductions in use of service: hospital admissions/re-admissions, length of hospital stay, and emergency department visits typically declined. It is important that there often were reductions in mortality. Few studies reported neutral or mixed findings.

|
Scooped by
rob halkes
|
Wearables are anything but sensible, from first hand observation they are somewhat silly, as they are trying to solve a problem that can be solved by a myriad of simpler and more passive mechanism. If you were at CES, you could not have missed a new category of computing called "wearables." This category of devices can be described as the FitBit gone mad. Wearables currently come in three main categories: health trackers, watches and glasses. In each of these categories some if not all devices are pivoting to solving the world's biggest health problems. Almost daily, I see a new wearable device launched, and while they all are minimally viable products, they continually get sillier and sillier. We are seeing everything from wearable necklaces (like necklaces were never wearable) earrings, shoes, clothing and many other bodily accruements being outfitted with small computers/biosensors, low voltage needs and high connectivity. Like clockwork, every new device no matter how silly, calls out to the world with press releases, tweets, YouTube videos and multiple pounds of the manufacturing firm's proverbial digital chest reckoning how disruptive some new wearable product is. My observation is that we have bastardized the word disruption. Most wearables are disturbing mankind under the once well-intended charter of disruption. While a minority of humans continue to wear these devices past the first few months of purchase, most folks (like myself) stop wearing after the nostalgia has worn off. I gave up my FitBit after about six months, my pebble watch in about six days and my Google GLASS, well I got over that bad boy in about six hours. I got over them the same way I got over my first CASIO watch, which doubled as a calculator in high school; said watch plus calculator was disturbing my life. Disruption does not have to disturb. Good disruption is change without disturbance. The hypothesis is simple, wearing something on my body that is not confortable, fashionable and delivering more value than it disturbs me is not a sustainable value proposition. So the big question is what will become of wearables? Clearly the movement of computing to the edge of the network will continue, and the connecting of things/biosensors that are not computers (Internet of Things) will continue. Wearables currently position themselves as trying to solve health's biggest problems. [..] Read the full article!

|
Scooped by
rob halkes
|
Editor's note: Matt Turck is a managing director of FirstMark Capital. The he emerging Internet of Things — essentially, the world of physical devices connected to the network/Internet, from your Fitbit or Nest to industrial machines — is experiencing a burst of activity and creativity that is getting entrepreneurs, VCs and the press equally excited.The space looks like a boisterous hodgepodge of smart hobbyists, new startups and large corporations that are eager to be a part of what could be a huge market, and all sorts of enabling products and technologies, some of which, including crowdfunding and 3D printing, are themselves far from established. The chart [..] is an attempt at making sense of this frenetic activity. From bottom to top, I see three broad areas – building blocks, verticals and horizontals:
Building Blocks The concept of the Internet of Things is not new (the term itself was coined in 1999), but it is now in the process of becoming a reality thanks to the confluence of several key factors. First, while still challenging, it is easier and cheaper than ever to produce hardware – some components are open sourced (e.g. Arduino microcontrollers); 3D printing helps with rapid prototyping; specialized providers like Dragon Innovation and PCH can handle key parts of the production process, and emerging marketplaces such as Grand St. help with distribution. Crowdfunding sites like Kickstarter or Indiegogo considerably de-risk the early phase of creating hardware by establishing market demand and providing financing. Second, the world of wireless connectivity has dramatically evolved over the last few years. The mobile phone (or tablet), now a supercomputer in everyone’s hand, is becoming the universal remote control of the Internet of Things. Ubiquitous connectivity is becoming a reality (Wi-Fi, Bluetooth, 4G) and standards are starting to emerge (MQTT). The slight irony of the “Internet of Things” moniker is that things are often connected via M2M (machine to machine) protocols rather than the Internet itself. Third, the Internet of Things is able to leverage an entire infrastructure that has emerged in related areas. Cloud computing enables the creation of “dumb” (simpler, cheaper) devices, with all the intelligence processed in the cloud. Big data tools, often open sourced (Hadoop), enable the processing of massive amounts of data captured by the devices and will play a crucial role in the space.
LinkedIn has become a staple social media outlet for professionals across the board, and now more than ever, people are actively using this platform to share information. One and a half million LinkedIn members are sharing content and sixty-five percent of users have increased their consumption over the past year. This drastic increase is now being called “the content revolution,” and is a phenomenon that should not go unnoticed by healthcare professionals.
The healthcare industry can take advantage of what marketers have already been doing and utilize these social media sites for digital marketing. LinkedIn recently released their 2014 Professional Content Consumption Report which surveyed over 2,700 users about their interactions with the site. As ninety-one percent of those surveyed list LinkedIn as their number one choice for professional content and the average user spends eight hours a week on LinkedIn, connecting with these content revolutionaries is an excellent way for healthcare professionals to network and share valuable insights and information.
Present novel information, or information that will assist in decision making. Fifty-six percent of users feel it is the easiest way to find professionally relevant content. Posts that present new and helpful information will be viewed and shared at a higher rate.
Use this platform to spark discussion. Fifty-one percent of users feel the main benefit of LinkedIn is the potential for sparking conversations. Content revolutionaries will share content that they feel evokes a response, and this content is more likely to be shared across other media platforms as well.
Ensure that sharing this content would benefit a user’s professional network. Sixty-two percent of users use LinkedIn to build relationships with colleagues or clients. Network building is one of the main draws of this platform, and content revolutionaries are likely to share information that aids in building relationships.
Format the content so it can be easily consumed on a mobile device. Users often need information at their fingertips and forty three percent of members visit this site on their mobile device.
Publish content that users want to share to enhance their professional brand. Some of the main benefits to using LinkedIn are that it increases member visibility, enhances a member’s professional brand reputation, and positions a member as an innovator. Content revolutionaries are most likely to share content that fulfills these needs.
For healthcare professionals to be most effective on LinkedIn, they must deliver information that content revolutionaries are seeking. In order to ensure that content revolutionaries share and consume healthcare professional’s content, it is important to present new, timely and discussion-worthy information.
Providing content beneficial to a professional’s network or brand, as well as providing small, easily “digestible” pieces of content will help increase the likelihood that the information is shared.
- See more at: http://scottpublicrelations.com/the-content-revolution-why-linkedin-is-ideal-for-healthcare-professionals/#sthash.8j1Uflgn.dpuf
Via Plus91

|
Scooped by
rob halkes
|
Philips, Salesforce.com and Radboud university medical center (Radboudumc) are collaborating to develop cloud based technologies to deliver better patient-centered clinical applications. Earlier this year, Philips announced its alliancewith CRM company salesforce.com to develop an open, cloud-based health platform integrating the data of medical devices and data from personal devices and offering applications. Philips at the same time announced the first two clinical applications to run on this platform that allow doctors and other caregivers to monitor patients with chronic conditions in their homes. REshape will be using this new Philips HealthSuite cloud-platform and its applications to further develop and implement its innovative patient services, creating an environment in which patients are equal partners in care delivery. Lucien Engelen, Director at REshape, says that in the past years, REshape has been actively experimenting with a number of innovative digital tools. The most ambitious of these is Hereismydata™, a combination of a personal health record, a community system for patients, caregivers and families and a connectivity tool for all kinds of medical devices and apps, fully embedded in the clinical process. “Our pilots and clinical trials made it clear that traditional hospital software does not offer all the required functionality to share device and treatment data in a secure way. Therefor the patients themselves should be able to own (at least a copy) of their own records. [...] Radboudumc is the first European academic hospital to use the new Philips HealthSuite platform for actual clinical usage. One of the first pilots will be patients with the chronic condition COPD. They will be monitored with devices such as the Health Patch, a small sensor worn on the chest that enables clinical-grade remote monitoring. Pilots involving patients with heart disease, diabetes and pregnancy will follow in the next months. “We are witnessing an explosion of personal medical data”, Engelen says, “but the real challenge is to integrate this data in the systems that doctors and other caregivers are actually using in their day-to-day processes and to make sure that doctors and patients can trust the data.” ...

|
Scooped by
rob halkes
|
Madison, Wisconsin-based Propeller Health, formerly known as Asthmapolis, has raised $14.5 million in a round of funding led by Safeguard Scientifics with participation from return backer The Social+Capital Partnership. (..) The smart inhaler company’s devices and companion apps offer geographic mapping of inhaler use and asthma triggers as well as adherence tracking and early warning alerts for COPD patients. “The funding supports the mission we are already on: to bring sensors to the full variety of the inhaled medications that are used for chronic respiratory disease,” Propeller Health CEO David Van Sickle told MobiHealthNews in an interview. “We are already well down that path… but the respiratory pipeline is fairly active. We are seeing new medications, therapies, and form factors.” In May Propeller received FDA clearance for its COPD offering. The new platform aims to help users prevent so-called “asthma attacks” or similar lung inflammation symptoms caused by COPD. The Propeller Metered-Dose Inhaler measures a patient’s use of their rescue inhaler. That data is automatically compared to a patient’s baseline and to general clinical guidelines, and the app can alert care teams if an attack seems likely. “In addition software development, as we take on more COPD programs, we have a broad spectrum of demographics that we have to cover with our products and services,” Van Sickle said. “So we are building out teams to support the usability and experience of not only kids with respiratory disease but elderly folks with respiratory disease, caregivers, new enterprise teams for care managers which are on their own evolving with the times and new healthcare arrangements.”(..) Propeller is seeing a lot of interest in COPD programs, Van Sickle said, partly driven by the market forces in healthcare incentivizing providers to reduce readmissions for COPD patients in particular. (..)

|
Scooped by
rob halkes
|
New Evidence Points to Outcomes and Cost Benefits of Telemedicine in Managing Chronic Diseases
New Rochelle, NY, September 10, 2014 Congestive heart failure, stroke, and chronic obstructive pulmonary disease (COPD) are three of the leading causes of death in the U.S. The use of telemedicine to help manage chronic diseases such as these can yield clear benefits including fewer and shorter hospital stays, fewer emergency room visits, less severe illness, and even fewer deaths, as reported in a study published in Telemedicine and e-Health, a peer-reviewed journal from Mary Ann Liebert, Inc., publishers. The article is available free on the Telemedicine and e-Health website until October 10, 2014.
Rashid Bashshur, PhD, Gary Shannon, PhD, and Brian Smith, MS, led a team of clinicians and researchers from the U.S. and Canada that included Telemedicine and e-Health Co-Editors-in-Chief Charles R. Doarn, MBA, and Ronald C. Merrell, MD, in the study entitled “The Empirical Foundations of Telemedicine Interventions for Chronic Disease Management.” The advantages enabled by telemedicine derive from its ability to help patients become more involved in their own care, facilitate continuous monitoring and early detection of new and recurring symptoms, and allow for prompt responses to worsening illness.
“The integration of telemedicine into healthcare adds great value in managing chronic disease both for patient and provider,” says Co-Editor-in-Chief Charles R. Doarn, MBA, Research Professor of Family and Community Medicine, University of Cincinnati, Ohio. “Dr. Bashshur has presented this work to both the U.S. Congress and the Congressional Budget Office, and with concomitant efforts by the American Telemedicine Association and others, the Congress may finally move telemedicine forward as an important element in healthcare for all Americans.
|





 Your new post is loading...
Your new post is loading...
























Goes without saying. Apple's "Healthkit" amazing. Bringing health parameter data together, AND aligning and integrating these with some of us, like the Mayo clinic, while RadboudUMC was mentioned too.
Now, as "traditional health care providers", we are in to the competition with Samsung and Apple regarding health care. But through them with selected health care providers, as well. These might get first response privileges from Apple: responding to customers worries about their data, even facilitate "preemptively" responding without being asked, to users with alerts, or ".. you better connect with us" - messages.
Imagine how disruptive that is..
Are you shocked? Well this is what was immanent. But there are angles that are still rather easy to overcome.
For instance, Apple's application seems to be still a hub, instead of an integrated platform: that is, it connects and relates, also even provides interaction facilities, but it will still be the same image of my iPhone with all its apps.. It is not (yet) an integrated ehealth platform.
There are your opportunities.
In this frame, I might say: it's my alert to you: get in touch, see my email here ;-)